CHILD HEALTH
HAEMATOLOGY
NUTRITION
Iron deficiency: The developing child at risk
Iron deficiency remains a common condition in children, with research suggesting many negative effects on the developing child
March 1, 2013
-
Iron deficiency is the most common and widespread nutritional disorder in the world.1 The World Health Organisation (WHO) estimate that iron deficiency accounts for 40-50% of anaemia in children and up to 80% in preschool children (2-5 years old) worldwide.1 High-risk groups for iron deficiency have been identified as preterm infants, children aged 1½-3½, and girls aged 11-18 years.2
Irish research shows that iron intake is a concern among all age groups. These concerns are outlined below:
Infants
At birth, an infant is endowed with iron stores. These usually become depleted within the first four to six months of life. A number of factors determine the rate of depletion, eg. infant stores at birth are highly related to maternal iron stores.3 Bioavailability of iron in breastmilk is high and formula milks are fortified with iron, however, milk alone will not be sufficient to meet iron requirements in the latter half of the first year of life.
Studies on iron status in infants are limited but research suggests that in Europe (including Irish data) 7.2% of infants at 12 months old are iron deficient with 2.3% having iron deficiency anaemia.4
Pre-schoolers
The National Preschool Nutrition Survey 20125 found that 23% of one-year-olds, 10% of two-year-olds and 11% of three-year-olds were estimated to have inadequate iron intakes. The main dietary contributors across all one- to four-year-olds were breakfast cereals, with milk/formula intake reducing with age and bread intake increasing with age. Meat products provided 11% of iron intake across all one to four-year-olds.
Children
The National Children’s Food Survey 20056 reports that one-third of girls between the ages of five and 12 years (34%) had inadequate intake of iron and 13% of boys in the same age group had inadequate intake. The study reported that almost a third of daily iron intake was eaten at breakfast, with ready-to-eat breakfast cereals being the main contributor.
Teens
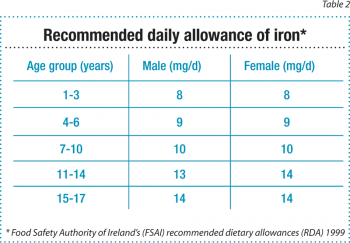
The average intake of iron for boys aged 13-17 years was 14.1mg/day and for girls aged 13-17 years was 10.7mg/day, according to the National Teens Food Survey 2006.7 This suggests that 13-17 year old boys are meeting 100% of their requirements for iron, while on average 13-17 year-old girls are meeting only 76% of their daily iron requirements.
Consequences of iron deficiency in children
Iron is an essential nutrient. It is a component of haemoglobin and myoglobin which transport and store oxygen around the body. It is also a component of many enzymes which are involved in the metabolism of energy and protein.2 Requirements for iron are highest during periods of rapid growth due to its role in cell development. Therefore, children are at greater risk of iron deficiency than full grown adults.
Iron deficiency results in defective erythropoesis leading to a normocytic or microcytic hypochromic anaemia. Studies suggest that iron deficiency anaemia is a cause of poor motor development in children in the first three years of life. This may be explained by the role of iron in brain development or may be due to behavioural issues.
The amount of iron in the brain increases throughout childhood and early adult life. Suggested roles of iron in the brain include a role in myelin sheath production and acting as a catalyst in the synthesis of neurotransmitters such as dopamine and serotonin. It is thought that iron deficiency may impair certain pathways and this may be a cause of cognitive impairment. Another potential role is the functional isolation which can be associated with iron deficiency due to symptoms such as poorer concentration and less energy to move around and play, thereby reducing cognitive stimulation.
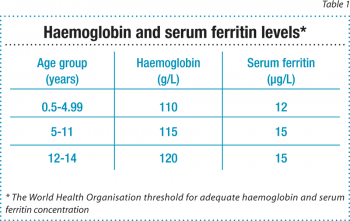
In older children, iron deficiency is thought to effect cognitive development, with studies suggesting that treatment of iron deficiency in this age group (older than three years) can improve school achievement.2 However, the long-term implications of these findings are unknown, as are thresholds at which these complications occur. The aim would be to maintain iron stores within the range outlined by the WHO (see Table 1).
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)