NUTRITION
Person-focused approach to dysphagia care
Since 2012, an initiative has been underway to develop standardised terminology for texture modified foods and fluids used in the management of dysphagia
September 28, 2016
-
The International Dysphagia Diet Standardisation Initiative (IDDSI) is a group of healthcare professionals who, in 2012, voluntarily came together from around the world to work collectively to develop internationally recognised, standardised terminology and definitions for texture modified foods and fluids used in the management of dysphagia.
The group is made up of representatives from diverse fields such as nutrition and dietetics, medicine, speech and language therapy, occupational therapy, nursing, patient safety, engineering, as well as food science and technology.
Objectives
The objectives of the IDDSI are as follows:
• To develop a standardised way of naming and describing texture modified foods and thickened liquids for people with dysphagia across the lifespan
• Their process is intended to be person-focused, rather than profession-focused. They seek to develop a global terminology that will ‘work’ for all cultures and that will be accompanied by practical and valid measurement techniques that will facilitate use by persons with dysphagia, caregivers, clinicians, food service professionals and industry partners
• To seek a common language that can be used for technical, cultural, professional and non-professional uses. The IDDSI believes this should be a living document, changing as needs change.
IDDSI framework
The IDDSI framework and supporting descriptor and testing methods documents were completed and published in November 2015.
In response to the global community, the IDDSI board has agreed to lead and co-ordinate IDDSI implementation.
Here in Ireland, many dietitians will be familiar with IDDSI’s national texture descriptors for foods and fluids, which were adapted from Australian guidelines by a working group made up of representatives from INDI and the Irish Association of Speech and Language Therapists (IASLT) back in 2009. A review of this document was overdue so with the publication of the IDDSI framework document, it seemed timely to initiate that review earlier this year.
Members of the INDI representing acute hospitals (Aisling McHugh, clinical specialist dietitian, St James’s Hospital, Dublin – group chair); paediatrics (Amy Craddock, paediatric dietitian, Children’s University Hospital, Temple Street, Dublin); disability (Mairead O Sullivan, senior dietitian, Early Intervention Services Waterford); and community and older people services (Siobhan Quigley, community dietitian, HSE West) came together in Dublin last April with members of the IASLT to meet with IDDSI co-chairs, Peter Lam, dietitian and credentialed food service executive, Vancouver, Canada, and Julie AY Cichero, speech and language therapist specialising in dysphagia research, Australia.
The aim of the meeting was to receive a full overview of the IDDSI framework and how it related to our existing national descriptors. The goal was to then examine if it would be prudent for us in Ireland to adopt the IDDSI framework for the management of dysphagia or to proceed with a standard review and update of the existing Irish guidelines.
The final dysphagia diet framework consists of a continuum of eight levels (0 to 7), where drinks are measured from levels 0-4, while foods are measured from levels 3-7.
IDDSI descriptors
As are evident in Figures 1 and 2, the new IDDSI descriptors are very similar to those already in use here in Ireland. The only difference to terminology will be that texture C smooth pureed foods are to be referred to as ‘level 4 puréed food’ and grade 1 fluid, very mildly thick, is to be referred to as ‘level 1 slightly thick’.
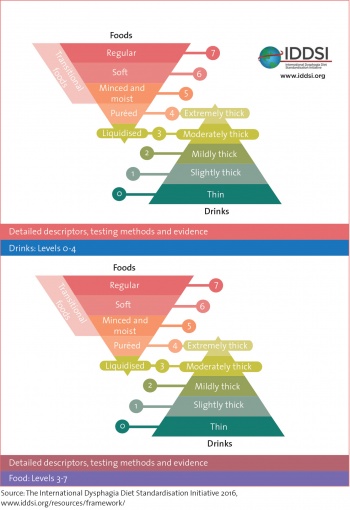 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)