ENDOCRINOLOGY
Update on bariatric surgery options for obesity
While bariatric surgery requires initial economic investment, it has been shown to be cost effective due to reduction and amelioration of long-term comorbidities of obesity
January 3, 2017
-
Nearly One-quarter of the Irish population is now classified as obese with a 1,200% increase in the number of Irish people with a BMI over 50 in the past 30 years. Bariatric surgery is the most effective treatment for morbid obesity leading to sustained weight loss and control of comorbid conditions.1 Bariatric surgery dates back to the 1950s when Kremen and Linner introduced the jejunoileal bypass, the first effective surgery for obesity in the US. Since then our BMI as a population has surged and along with it the development of diverse and elaborate procedures to try to counteract our ever growing waist band.
Despite this, rates in Ireland remain low with less than 100 procedures performed in the past year – when the estimates are that more than 80,000 Irish people are eligible for the surgery and that 40,000 would be open to having a surgical procedure to aid weight loss.
Indications for bariatric surgery include:
- Adults with BMI ≥ 40kg/m2
- Adults with BMI ≥ 35-39.9kg/m2 with at least one serious comorbidity, eg. type 2 diabetes, obstructive sleep apnoea, hypertension, hyperlipidaemia
- Adults with BMI 30-34.9kg/m2 with uncontrollable type 2 diabetes or metabolic syndrome.
Bariatric surgery is based on two fundamental mechanisms, restriction and malabsorption. Restrictive procedures limit food intake by reducing the stomach’s reservoir capacity. Malabsorptive procedures reduce absorption of nutrients by shortening the length of functional small intestine. Some procedures work via a combination of restriction and malabsorption.
The trend in type of surgeries performed has changed over the years. Gastric banding was previously the favoured procedure followed by gastric bypass and bilio-pancreatic diversion. In recent years sleeve gastrectomy has joined the gastric bypass as a more popular procedure and gastric banding has become much less frequently performed.
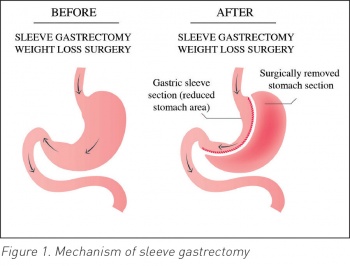
Sleeve gastrectomy
Laparoscopic sleeve gastrectomy (LSG) is a partial gastrectomy, in which the majority of the greater curvature of the stomach is removed, creating a tubular stomach. It is a restrictive procedure but also has effects on gastric motility and gut hormones, including ghrelin which plays a role in the stimulation of appetite and gastric motility.2,3
Sleeve gastrectomy was originally carried out as a first stage procedure followed by laparoscopic Roux-en-Y gastric bypass (RYGB) or duodenal switch but has become increasingly popular as a single stage laparoscopic procedure.4 It is considered easier, faster and less traumatic compared to RYGB.
Advantages include preservation of endoscopic access to the upper GI tract, normal absorption, lack of intestinal anastomosis and complications due to anastomotic leak. The pylorus is also preserved preventing dumping syndrome.
A recent randomised control trial comparing LSG to RYGB showed that they were equally safe and effective at one year follow-up with regard to weight and reduction and amelioration of comorbidities.5 LSG had an excess weight loss (EWL) at six and 12 months of 64.2% and 67.6% respectively. A total of 75% of patients achieved an EWL of > 50% at one year post op.5
Reported complication rate with LSG is variable with one study showing only a 2.9% major complication rate.6 However a study of patients having LSG as an initial procedure prior to a gastric bypass showed a complication rate of 14%. The majority of complications were noted to be self-limited and the cohort of patients in this study may have been premorbidly at higher risk than in other studies with an average BMI of 65.4 on enrolment.7
Complications include haemorrhage from gastric vessels or staple line, stricture of the created tube, gastric leak, splenic injury and late stenosis and gastroesophageal reflux. Patients are also at risk of micronutrient deficiency, and regular testing of iron, B12, vitamin D and calcium is recommended.4 The first report from the American College of Surgeons Bariatric Centre network shows that the mortality rate of LSG is 0.11% at 30 days and 0.21% at one year placing it between RYGB and laparoscopic adjustable gastric banding (LAGB).8
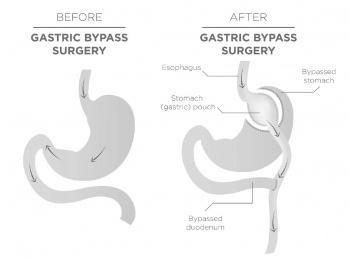
Gastric bypass
Roux-en-Y gastric bypass works by both restrictive and malabsorptive mechanisms. It involves the creation of a small gastric pouch by dividing the upper end of the stomach. The small intestine is then divided and a ‘Roux’ limb is anastomosed to the gastric pouch, creating a small reservoir and restricting caloric intake. A biliopancreatic limb of small intestine is also created transporting secretions from the gastric remnant, liver and pancreas and the two limbs are then connected forming a common channel where digestion and absorption of nutrients occur. Increasing the length of the Roux limb can increase malabsorption. Most RYGB are now performed laparoscopically.
RYGB also affects gut hormones, ghrelin levels are reduced and glucagon-like peptide 1 (GLP -1) levels are increased.3 GLP-1 is an incretin released from entero-endocrine cells which can inhibit gastric emptying and reduce food intake. Levels of peptide YY, a gut hormone that reduces appetite, have also been shown to increase after RYGB.3
Excess weight loss ranges from 64-69% at 12 months and 83% at 24 months with most obesity-related complications eradicated or improved.5,9 A recent study comparing RYGB with gastric banding showed substantially greater weight loss and lower fasting blood glucose and cholesterol levels with RYGB.10 Early complications include peritonitis, bowel obstruction and anastomotic leaks and later complications include gastric remnant distension, stomal stenosis, marginal ulcers, cholelithiasis, incisional hernias, dumping syndrome and metabolic and nutritional derangements. Major complication rates have been reported at 3.3%.9 A recent study showed a 2.1% rate of long-term complications requiring corrective procedures compared with 8.9% in those who had LAGB.10 Mortality rates at 30 days and one year are reported to be 0.14% and 0.34% respectively.8
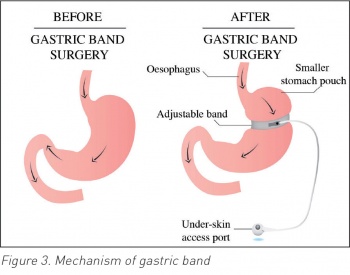
Gastric band
Adjustable gastric banding is a restrictive procedure in which an adjustable prosthetic band is placed across the top portion of the stomach. This creates a small pouch with limited volume, inducing early satiety and reduction in caloric intake. An infusion port is placed in the subcutaneous tissue allowing injection of saline to adjust the band diameter. The band also slows passage of food to the lower part of the stomach, leading to decreased food intake and subsequent weight loss. This can be performed as an open surgery but is most commonly performed laparoscopically. Gastric banding is a relatively safe and simple procedure as it does not involve division of the stomach or intestinal resection. The adjustability of the outlet also offers the advantage of being able to address nutritional issues following surgery.
Irrespective of pre-operative BMI, LAGB has been shown to cause less weight reduction than RYGB.10 However, LAGB had been shown to be a safe procedure with a low rate of acute complications (0.5% in LAGB, 8% with RYGB).10 Acute complications include small leaks requiring band removal and wound haematoma formation. LAGB also has impressive long term follow-up data with an EWL of 47% maintained to 15 years.11 Although the need for revisional procedures has decreased in recent years, 15 year follow-up data showed that almost half the patients required one or more follow-up procedures. The reasons for additional surgical procedures include need for enlargement of the band, erosions, changed in tubing or replacement of the band.11 Having initially increased in popularity at the start of the 21st century, its success has been superseded by the gastric sleeve which is increasing in prevalence.12
Biliopancreatic diversion with duodenal switch (BPD/DS)
This is now only performed in a few centres in the US and has largely been replaced by the procedures described above. A sleeve gastrectomy is created. The small bowel is divided at two points – the duodenum and mid jejunum. The most distal jejunal and ileal loop are brought up to reconnect to the stomach and duodenum, bypassing the biliary and pancreatic drainage. The excluded aspect of the duodenum and jejunum is reattached to the distal portion of the small bowel loop to allow drainage of biliary and pancreatic fluid.
It is a combination of restrictive and malabsorptive weight loss mechanisms with some effect on gut hormones, although this is poorly studied. A retrospective study done in 2012 showed that BPD/DS was associated with longer operative times, greater blood loss and longer length of stay compared to gastric bypass, however percentage change in BMI and control of comorbidities was significantly greater with BPD/DS.13 Bowel obstruction is the most common complication, with one study showing a 16% incidence of same.14
Novel therapies
Novel therapies that are being investigated to treat obesity include an ‘endobarrier’ and a venting gastrostomy. An endobarrier involves placing a barrier device extending from the proximal duodenum to the mid jejunum, preventing luminal contents being absorbed. However, it can be poorly tolerated and has a high rate of early device withdrawal due to same.15 The venting gastrostomy involves a reverse PEG tube that allows food to be emptied from the stomach 20 minutes to half an hour after it has been consumed.
Long-term follow-up
As well as physical effects of the surgery in recent years the psychiatric sequelae of bariatric surgery have come to light. A cohort study carried out in Canada on a large number of patients post bariatric surgery showed a significantly increased risk of self-harm emergencies post bariatric surgery.16 Most of these emergencies happen in the second and third year postoperatively, when the period of substantial weight loss comes to an end.17 This emphasises the need for long-term follow-up post bariatric surgery especially in those with a prior history of depression and/or self-harm.
Conclusion
LSG is now the most popular bariatric procedure given its effectiveness in achieving weight loss along with a low risk of complications and relative simplicity. A prospective study of bariatric surgery databases in the US was carried out comparing RYGB, LSG and LAGB. It showed that LSG has higher 30 day-morbidity, readmission and reoperation/intervention rates compared to the band, and lower reoperation/intervention rate compared to the bypass. The study showed that the absolute reduction in BMI following the LSG is less than the weight loss following the LRYGB/ORYGB but greater than the weight loss after the LAGB.8 However, this study was somewhat limited by the number of LSG cases with one year data available and as the popularity of LSG continues to grow longer-term data will become available for LSG and shine further light on its longer term advantages and disadvantages.
Bariatric surgery requires initial economic investment but has been shown to be cost effective due to reduction and amelioration of long-term comorbidities of obesity. However, in the midst of new and advanced surgical techniques being developed, one must not forget that obesity is a preventable disease. These surgeries have been developed due to an overwhelming need following a change in our eating habits and activity levels in the past century. Preventing obesity from a young age must become a priority in our health system. We have sophisticated surgical solutions for the problem that obesity is, however let us not forget why the problem first arose.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)