DIABETES
Glucose control – are we forgetting a big part of the story?
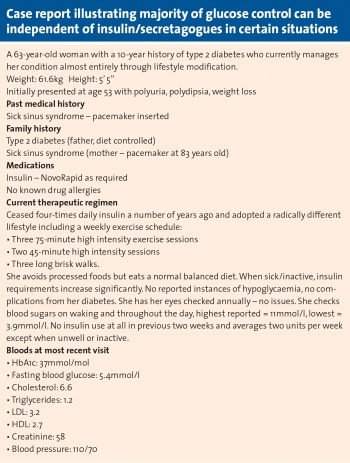
As the understanding of glucose metabolism continues to improve, it appears there may be an overreliance on insulin as a therapeutic modality
December 11, 2015
-
Insulin is widely considered to be the most significant contributor to glucose homeostasis and consequently insulin remains a primary treatment for blood glucose regulation. However, in the fasting state, over 80% of glucose handling occurs via non-insulin mediated glucose uptake.1 This definition is somewhat dismissive as it categorises a broad spectrum of glucose disposal as merely ‘non-insulin mediated’ and furthers the myth that insulin is essential for the majority of glucose uptake/metabolism.
Research and understanding about how the body handles glucose has dramatically increased over recent decades (with a puzzling lull in the 1990s). We now understand that glucose itself plays a substantial role in its own metabolism. ‘Glucose effectiveness’ refers to the ability of hyperglycaemia to promote glucose disposal at basal insulin levels by both increasing glucose uptake into cells, and decreasing hepatic glucose production.
The glucose effectiveness and non-insulin mediated glucose uptake pathways vary in their contribution to blood glucose depending on the individual’s metabolic state. For example in the setting of insulin resistance, non-insulin mediated glucose uptake increases and becomes of greater importance to glycaemic control than in an insulin-sensitive individual. Similarly glucose effectiveness, while estimated to contribute to 50% of glucose disposal in healthy subjects, rises to as much as 80% of glucose regulation in obese insulin-resistant individuals.2
A decrease in glucose effectiveness is closely associated with the onset of type 2 diabetes, with endogenous glucose production persisting in the presence of an elevated blood glucose level and perpetuating the vicious cycle of hyperglycaemia.3,4 Metformin’s primary mode of action is to restore glucose effectiveness by suppressing hepatic gluconeogenesis.
Drivers of insulin resistance
High levels of plasma free fatty acids (FFAs) – driven by obesity and high fat diets – are now established as drivers of insulin resistance.5 We now understand that FFAs disrupt the hepatic processes that would normally respond to hyperglycaemia thus reducing glucose effectiveness.6 This mechanism initially elucidated in mouse studies has been dramatically supported by the complete restoration of glucose effectiveness in human subjects following the normalisation of plasma FFA levels.7,8
While medical practitioners have for years been preaching the virtues of ‘diet and exercise’ as the cornerstone of type 2 diabetes management, there has not been a good mechanistic understanding to underpin that advice. There is now good evidence for the improvement of glucose effectiveness in response to moderate exercise.9
The Glut system
The ‘glucose transporter’ (Glut) system is a series of cell surface proteins (over 10 identified so far) that shuttle glucose in and out of cells. Even Glut 4 – the most closely associated with insulin – has been demonstrated to facilitate glucose uptake in response to nitric oxide stimulation independent of insulin secretion.10
This is one of the mechanisms by which insulin-independent uptake is increased after exercise. In this case the normally insulin-dependent pathways undergo significant adaption to operate independently of the hormone. These changes take place in the peripheral tissues where uptake occurs, namely adipose tissue and skeletal muscle.11
Emerging role of the brain in controlling blood glucose
There is growing evidence that supports a significant role for the hypothalamus mediating insulin-independent glucose disposal.12 This is a concept that is already being explored as a potential pharmacological avenue alternative to insulin-based strategies.13
The hormone fibroblast growth factor 19 (FGF19) is currently central to this idea of the brain as performing a dynamic role in insulin-independent glucose homeostasis. Analogues of FGF19 are currently being developed for human use.
FGF19 is produced by the terminal ileum in response to bile acid absorption there. The hormone plays a role in glycogen and protein synthesis as well as the inhibition of gluconeogenesis – in other words increasing glucose effectiveness. This has been suggested as a mechanism for the remission of type 2 diabetes post bariatric surgery (gastric bypass) where FGF19 levels have been shown to normalise.14,15
The next 10 years will bring a much more detailed understanding of this gut-brain axis and its role in weight and glucose regulation.
At present, insulin-based strategies remain the cornerstone of treatment for diabetic hyperglycaemia. Either by direct administration of exogenous hormone or pharmacological stimulation of endogenous production/sensitisation we rely greatly on insulin-dependent means of regulating glucose homeostasis.
As our understanding of glucose metabolism continues to improve it appears as though there may be an overreliance on insulin as a therapeutic modality. The latest research would suggest that we may be struggling to control a condition while utilising only 30-50% of the tools at our disposal.
 (click to enlarge)
(click to enlarge)
