CANCER
CHILD HEALTH
MENTAL HEALTH
Integrated psychosocial care of children with advanced cancer and their families
Described in this article is the impact of symptom distress on children with advanced cancer and their families
July 20, 2019
-
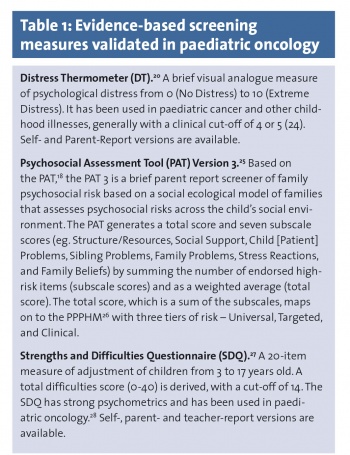
The benefits of timely and appropriate referral to paediatric palliative care are named. The merits of systematic identification of psychosocial risk are given. Finally, an example of an integrated model of psychosocial care is presented by reference to work ongoing at LauraLynn Ireland’s Children’s Hospice.
Symptom distress and quality of life
Each year in Ireland approximately 210 children under the age of 19 are diagnosed with cancer with the majority surviving beyond five years.1 Despite increasing survival rates, these children remain at risk for high symptom distress.2,3,4 Common physical symptoms associated with distress among children with advanced cancer are pain, fatigue, and drowsiness, whereas irritability and sleep disturbance are highly distressing psychological symptoms.4 The effect of these symptoms is to diminish the child’s quality of life.5,6,7
Family psychosocial risk
For parents, the stresses associated with the carer role are numerous. Examples include co-ordinating and delivering medical care, decision making, communication with professionals and within the family, containing distress, disruption to family roles and routines, financial costs, and the prospect of losing the child.8 Difficulty adjusting to the role as carer is expressed as problems with mood, disturbance of sleep, fatigue, and feelings of fear in relation to the child’s symptoms and the prospect of the child dying.9,10
The experience of caring for a child with cancer also places strain on spousal relationships11 and relationships within the extended family.12 With respect to siblings’ psychosocial adjustment to childhood cancer, symptoms of cancer-related post-traumatic stress are prevalent, as is poorer academic functioning and greater absenteeism.13
End-of-life and palliative care
A subgroup of children with cancer succumb to their illness, with an average of 24 deaths occurring in Ireland per year due to childhood cancer.1 At the end of life, the most frequent and problematic symptoms are pain and fatigue, occurring in almost all children.10,14 Feelings of sadness, anxiety, irritability, and a range of distressing physical symptoms also feature.2,3,15
Timely and appropriate referral to palliative care services is one way of offsetting some of the burden on the child and family.8 Referral to palliative care is linked with improved parental perceptions of children’s symptoms, enhanced quality of life and communication, better family support, and greater co-operation between families and healthcare providers.16 Children who receive palliative care also spend fewer days in hospital, receive fewer invasive treatments, and are less likely to die in the ICU.17
Psychosocial care pathways
Just as there are obstacles to achieving integrated medical care of children with cancer so are there difficulties in relation to the delivery of psychosocial care to seriously ill children and their families. Psychosocial supports are typically not provided in a systematic or consistent way across or within paediatric oncology settings.18 Recognising this, the interdisciplinary team at LauraLynn Ireland’s Children’s Hospice (‘LauraLynn’), an organisation that provides hospice and palliative care to children with life-limiting illnesses, including certain cancer diagnoses, developed a pathway which allows for mutual decision-making and organisation of psychosocial care processes that are aligned with best practice. The pathway is adhered to by all staff in order to ensure high standards of equitable and sustainable psychosocial care.
Screening and referral of psychosocial risk
As per the psychosocial care pathway, concerns are flagged in the course of routine screening and, more organically, arising from staff contacts with the child and family members or in the form of external- or self-referrals. In respect of routine screening of psychosocial risk, a semi-structured clinical interview known as the Holistic Needs Assessment (HNA) is carried out with each family at point of admission to the service. Developed by a cross-section of professionals at LauraLynn, the HNA captures data on the child and family across five domains. In addition to detailing the child’s physical needs, it collates information relating to the child and family’s psychological/emotional wellbeing, social factors, spirituality, and the child’s adaptive skills (eg. communication, play/leisure, managing routines, learning). At LauraLynn, the most commonly identified care goals, in order of prevalence, are those relating to the child’s physical needs, child and family psychological/emotional needs, and the child’s adaptive behaviours.19 In addition to the HNA, annual reviews are carried out, which take stock of both the child’s care needs and the broader needs of the child and family.
Responding to psychosocial risk
At the time of writing this article in June 2019, to augment data collated from HNAs and annual reviews, and to allow for clear identification of psychosocial concerns as they arise over time, the team at LauraLynn have integrated into the care pathway a system of referral that is tailored specifically to a children’s hospice and palliative care setting. A brief psychosocial referral form invites the referrer to describe what the main concerns are, what supports have been accessed/helpful to date, and it incorporates a standardised measure of distress known as the ‘distress thermometer’.20
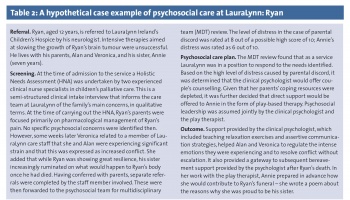
The information collated by the referral form is then processed systemically in a designated weekly forum by an interdisciplinary team. In this context, consideration is given to, among other things, what is the level of distress caused by the concerns, what offering will achieve the greatest gain, and who is best placed to assume psychosocial leadership of the case? This system provides for evidence-based psychosocial triage so that the team’s resource allocation is purposeful, and responsive to the type and severity of need21 (see Table 1 for examples of screening measures).
 (click to enlarge)
(click to enlarge)