CANCER
NURSING
Nurse-led telephone follow-up: reducing oncology outpatient waiting lists
Nurse-led telephone follow-up of oncology patients streamlines patient care from hospital to community by making the nurse accessible to the patient in the comfort of their own home.
May 1, 2012
-
Individuals who have been diagnosed with cancer require frequent follow-up in order to detect recurrent disease and manage the physical and psychological impact of treatment. The US National Cancer Comprehensive Network (NCCN) guidelines direct that these patients attend oncology outpatient clinics, often at frequent intervals, despite evidence in the literature showing that routine follow-up with clinical examination does not contribute to improved survival.1-4 The frequent follow-up visits of these patients in the outpatient clinic has a significant impact on the oncology service and requires continuous management.
Background
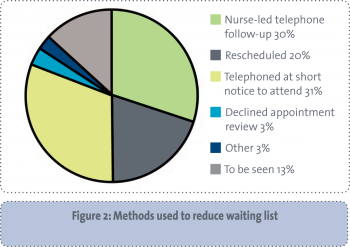
In Letterkenny General Hospital, in April 2010, it was identified that there were 177 patients on the oncology outpatient waiting list – a number that was growing every month. The oncology team discussed various methods to allocate appointments to these patients to expedite their review. One method that was identified and seemed possible was nurse-led telephone follow-up (NLTFU).
Literature review
Patient acceptability and satisfaction with nurse-led follow-up is consistently high in the literature.5-7 Additionally, NLTFU has often been portrayed as a positive and cost-effective means of follow-up. Cox et al, in their study of NLTFU in ovarian cancer, found that the majority of women expressed a preference for NLTFU; the main advantages were reported as the relationship and discussions between the patient and the nurse, and the convenience of having follow-up appointments by phone rather than attending clinic.8
Beaver et al conducted a study exploring the views of patients and nurse specialists involved in telephone follow-up after treatment for breast cancer. The study reported positive views on this method.9 The researchers concluded that an experienced and skilled practitioner with effective communication skills was required to deliver the intervention and a period of training was recommended.
Cusack and Taylor found that telephone follow-up meets patient satisfaction, support and information needs, and has the potential to deliver high standards of aftercare when conducted by a nurse specialist.10 Additionally, they concluded that the option of telephone follow-up could, for some patients, dramatically improve their care experience. This finding was also reflected in a study by Kimman et al.11
Similarly, Beaver et al found that high levels of satisfaction with the care and delivery by colorectal nurse specialists, and patient acceptance of telephone follow-up, suggest that NLTFU is a viable alternative to traditional hospital-based follow-up.12
Kimman et al have identified that NLTFU plus a short educational group programme is an appropriate and cost-effective alternative to hospital follow-up for breast cancer patients during their first year after treatment.13 However, in a further study, they point out that an educational group programme does not unequivocally affect positive health-related quality of life outcomes. They concluded that NLTFU seems an appropriate way to reduce clinic visits and represents an accepted alternative strategy.14
Proposal development
Following a literature review, and identifying that NLTFU could be a safe and effective option for patient care, a proposal was written. This was developed in conjunction with Dr Karen Duffy, a medical oncologist at Letterkenny General Hospital. Her support as the clinical lead was a prerequisite for its introduction. Director of nursing and midwifery support was also secured prior to proceeding. Other nursing colleagues and medical secretaries were consulted to ensure that the practice change was appropriate and feasible.
The initiative was also discussed at the oncology senior management team meeting to obtain hospital management support. The completed proposal was submitted to the National Council for the Professional Development of Nursing and Midwifery (NCNM) to secure funding, which was successful.
Guideline development
The authors subsequently developed a guideline, which was to direct the holistic assessment for nurse-led telephone follow-up and to ensure that standardised practice and documentation were adhered to. Dr Duffy and other key stakeholders were consulted for their input into this document. It was subsequently ratified at the local nursing policy/guideline committee.
Patient inclusion/exclusion criteria for involvement in the telephone follow-up were identified and a standardised assessment sheet using Bickley recommendations for assessment was developed.15
The flow diagram (Figure 1) illustrates the comprehensive care for oncology patients participating in NLTFU. In addition, the decision was made to use the distressometer (www.NCCN.org) to assist patient assessment. It has been incorporated locally into a self-explanatory leaflet that encourages patients to focus on their needs. This leaflet was posted to patients along with the telephone appointment.
 (click to enlarge)
(click to enlarge)