ENDOCRINOLOGY
Anaemia referral
An audit was undertaken to evaluate when patients should be referred for endoscopic investigation of anaemia
September 1, 2013
-
The aim of this audit is to evaluate the appropriateness of referral for gastroscopy and or colonoscopy to investigate anaemia (presumed iron deficiency anaemia [IDA]).
Subjects
Patients who have had endoscopic examination (gastroscopy, colonoscopy or both) to investigate anaemia at the endoscopy unit, St James’s Hospital, between October and December 2011.
Methods
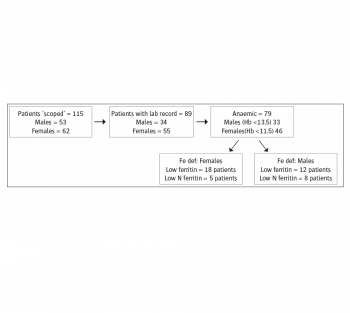
The endoscopy unit electronic data base (ADAM system) was searched for the term anaemia under indication drop menu in the minimum terminology system (MTS) for both gastroscopy and colonoscopy. The gastroscopy and colonoscopy data base were searched separately for the specified period. Running the statistics function for the months of October to December 2011 yielded 115 patients (62 females/53 males). The medical record number (MRN) and date of procedure for each patient were entered in an Excel spreadsheet.
Using the MRN the hospital electronic patients record (EPR) was searched and the index laboratory records (haemoglobin [Hb], mean corpuscular volume [MCV], ferritin, tissue transglutaminase [TTG], etc.) which prompted the referral for further endoscopic evaluation were identified and entered in the spreadsheet. This search also helped in classifying our cohort as inpatients or outpatients. The collected data were analysed using Excel and SSPS.
Results
Twenty-six patients were excluded because they have no laboratory records around the date of the index procedure(s) leaving 89 patients for final analysis (55 females/34 males), with the mean age of x (ranging from 28 to 97 years).
Seventy-nine patients (F=46/M=33) were anaemic as per our laboratory reference value for low normal Hb. Definite iron deficiency as defined by a ferritin of < 23 was seen in only 30 patients (F = 18/M = 12).There is a mismatch between the different indices of iron deficiency as low MCV was seen in just 50% of this group. Thirteen more patients had a ferritin in the lower normal range (24-50) and this acceptable indication for endoscopic evaluation.
Out of the total cohort of 89 patients, 60 (67.4%) had both gastroscopy and colonoscopy, 26 (29.1 %) had only gastroscopy and three (3.4%) had just colonoscopy to investigate their anaemia. Of all the patients who had an endoscopic investigation for anaemia, 33% (30/89) have definite evidence of iron deficiency or confirmed IDA. Endoscopic investigation was justified in an additional 13 patients on the basis of low normal ferritin (24 -50), bringing the final percentage of patients in whom endoscopic investigation was justified to 48%.
Discussion
In this audit only 48% of all patients who had an OGD and/or colonoscopy had a definite or probable IDA. Obviously the type of the anaemia and the iron status should be ascertained before embarking on invasive and potentially risky investigative procedures. However, this not always easy, particularly in anaemias of chronic diseases with or without concomitant Fe deficiency. Specific indicators of iron deficiency should be considered in such situations.
Recommendations
Ideally the referral form to investigate anaemia should detail Hb and ferritin levels and MCV. These are easily obtainable for in patients. The GP should provide these essential details as well as details of current or recent treatment with iron, folic acid and B12 supplements.
- Re-audit, after implementing these recommendations, starting first with inpatients.
- Standard, preferably, electronic referral forms for both inpatients and outpatients.
 (click to enlarge)
(click to enlarge)
