SURGERY
Triage to table: appendectomies performed in a regional hospital
An audit to determine whether significant delays were occurring between admission and appendectomy
March 24, 2014
-
Acute appendicitis is one of the most commonly encountered surgical emergencies today. Given the ubiquitous nature of the condition, however, it has also become one of the most commonly postponed surgical procedures.
Increasing the interval between emergency department (ED) admission and appendectomy has been shown to increase the development of advanced appendicular pathology, as well as increasing post-operative complications, length of stay and overall cost to the hospital service.1,2,3
Prior research in the mid to late 1990s suggested that a ‘wait and see’ approach could be beneficial for patients with suspected appendicitis,4 however more recent work has debunked this notion and has shown the importance of prompt treatment of this common yet significant surgical pathology.
Objectives
The objective of this audit was to determine whether significant delays were occurring between patient admission and appendectomy time. Furthermore we aimed to elucidate whether these delays, if any, were comparable to international figures.
Standard
No single international standard exists for the interval between admission and procedure in acute appendicitis. In this audit we used several relevant studies identified from the literature to produce a de facto standard. Through our literature review we observed a common finding that an interval time of greater than 24 hours2,3 from ED admission was a statistically significant predictor of poor post-operative outcomes. Some evidence suggests that 12 hours is the ‘watershed’ interval,1 but for this audit we have used an interval time of < 24 hours as our benchmark.
Complication rates were compared against reported figures from a 32,683-patient study by Ingraham et al,5 which reported a total morbidity rate of 4.5% for laparoscopic procedures and 8.8% for those performed following a laparotomy.
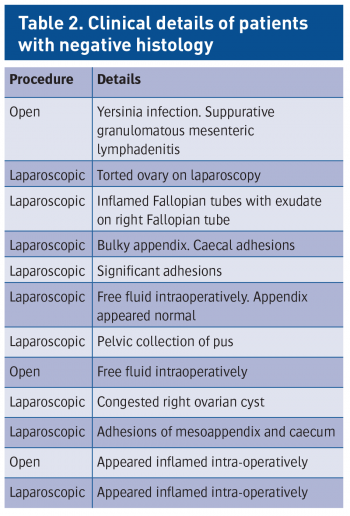
The rate of negative histology was measured against a paper by the SCOAP collaborative,6 which looked at 3,540 patients to review the rate of negative histology following either computed tomography (CT) or ultrasound (U/S) imaging. See Table 1 for a summary of these sources.
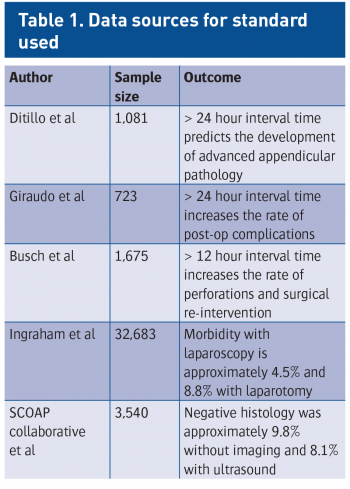 (click to enlarge)
(click to enlarge)