CARDIOLOGY AND VASCULAR
Heart failure in the community
Accurate heart failure diagnosis can help reduce hospital admissions and mortality and improve quality of life
November 1, 2011
-
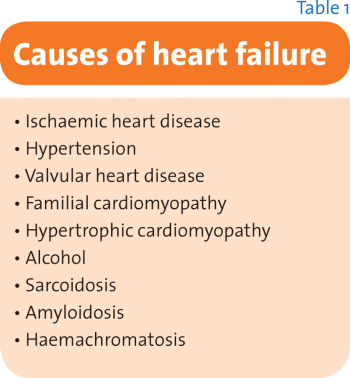
Heart failure is one of the major causes of morbidity and mortality in Ireland. It is a clinical syndrome consisting of symptoms such as dyspnoea and fatigue, signs such as elevated jugular venous pressure (JVP) and bibasal lung crepitations combined with objective evidence of cardiac dysfunction through testing such as echocardiography.1 Heart failure has a variety of underlying causes (see Table 1).
Heart failure has a mortality of 42% over five years.2 This is worse than with many forms of cancer. Much of heart failure is managed in primary care. It also frequently results in hospital admissions and readmission (25% of patients are re-admitted within 12 weeks of discharge3).
A GP with a practice population of 2,000 patients could expect to have 40-50 patients with heart failure. Fifteen new patients with suspected heart failure would be expected to present each year. Of these, five will have confirmed heart failure after diagnostic testing using methods such as echocardiography.4
The majority of patients with heart failure are elderly and therefore it is not surprising that 99.6% of patients with heart failure have comorbidities.5
Diagnosis
In the community, patients may present with symptoms that are vague or of slow onset, such as fatigue. Symptoms may also overlap with other conditions common in this age group, such as dyspnoea seen in COPD. Signs may be absent, or even misleading, such as ankle oedema, which is often due to other causes such as medications. Therefore it is not surprising that only 30% of patients referred to clinics with possible heart failure have this diagnosis confirmed following objective testing.6
Due to inability to access objective testing such as echocardiography it is performed infrequently. Only 34% of patients with a coded diagnosis of heart failure in the UK have had echocardiography.7
- Chest x-ray: Chest x-ray is most useful in determining if other causes of dyspnoea, such as pneumonia, are present
- ECG: A normal ECG means that the likelihood of heart failure is less than 10%. However, abnormalities such as left ventricular hypertrophy, atrial fibrillation or evidence of cardiac ischaemia may be evident
- Natriuretic peptide testing: This test is not widely available in general practice in Ireland at present but hopefully this should change. Brain-type natriuretic peptide (BNP) is a hormone secreted in the ventricular myocardium during periods of increased ventricular stretch and wall tension such as occurs in heart failure, hypertension, and myocardial ischaemia. Once secreted, the BNP precursor is split into the biologically active peptide NTproBNP. Testing is available for both BNP and NTproBNP. Both are equally sensitive and specific for heart failure, although they have different cut-off points for ruling out heart failure. NP levels may be raised in conditions such as heart failure, renal disease, atrial fibrillation, and ischaemic heart disease. NP levels are reduced by factors such as obesity, diuretics, ACE inhibitors and angiotensin receptor blockers.
Due to the fact that there are many causes of an elevated natriuretic peptide level, it is not useful in confirming the diagnosis of heart failure. However, a normal BNP or NTproBNP level combined with a normal ECG make such a diagnosis very unlikely and alternative causes for the symptoms should be sought.
Echocardiography
This is the most common test used to image the heart. From a heart failure perspective, two of the most important measures to take note of on echocardiography reports are left ventricular ejection fraction and left atrial size.
Left ventricular systolic function can be measured using a marker called left ventricular ejection fraction (LVEF). The LVEF is a measure of the amount of blood which is present in the left ventricle during diastole that is then pumped out of the left ventricle during systole.
The normal LVEF is 50-70%. The LVEF is also a marker of prognosis, with lower LVEF being associated with a worse prognosis.
Patients with heart failure and a reduced LVEF have been shown to benefit from treatments such as ACE inhibitors and beta blockers and are said to have heart failure with left ventricular systolic dysfunction (LVSD).
Filling of the left ventricle during diastole is another crucial component of cardiac function which is independent of LVEF. Simply put, if the ventricle cannot fill with blood then it cannot pump it out. It is influenced by left atrial pressure which drives filling of the left ventricle and left ventricle relaxation, which provides suction to draw blood into the ventricle.
Various markers of the diastolic function of the heart are used and may be commented on in echocardiogram reports. However, clinically significant diastolic dysfunction is uncommon without left atrial enlargement and this parameter should be looked for on echocardiography reports.
Patients with a normal ejection fraction but who have markers of diastolic dysfunction and symptoms and signs of heart failure are said to have heart failure with preserved ejection fraction (HFPEF). Patients with this condition do not have the same benefit from ACE inhibitors and beta blockers as patients with LVSD.
Possible causes for heart failure may also be elucidated during echocardiography, eg. valve abnormalities, left ventricular hypertrophy in hypertension, or abnormalities of ventricular wall movement in myocardial ischaemia.
The use of ECG and natriuretic peptide testing can effectively rule out the diagnosis of heart failure in general practice if both are normal. Echocardiography is an essential test in those patients who are being actively managed to confirm diagnosis and to help determine possible causes and appropriate medications for patients with heart failure.
Management of stable heart failure
The management of stable heart failure involves:
- Treatment of comorbidities which may exacerbate heart failure such as uncontrolled hyperthyroidism or COPD
- Treatment of cause of heart failure
- Promotion of self-care
- Avoiding medications which may exacerbate heart failure
- Use of treatments to improve morbidity and mortality in heart failure such as ACE inhibitors and beta blockers in LV systolic dysfunction.
Self care
Management of heart failure should be seen as a shared responsibility between patients, their carers and healthcare professionals. Improved self-care has been associated with improved outcomes in heart failure.
Weight reduction
Weight reduction in obese people with HF should be considered in order to prevent the progression of heart failure, decrease symptoms, and improve well-being.
Smoking
Smoking should be strongly discouraged in all patients with heart failure irrespective of aetiology. Non-smokers with heart failure (never-smoker or ex-smokers) have a 30% lower mortality compared to current smokers with heart failure.8
Alcohol
For those with cardiomyopathy related to alcohol, complete abstinence is advised. For others, moderate alcohol consumption is advised.
Exercise
Physical inactivity is common in patients with heart failure and contributes to its progression. Regular, moderate daily activity is recommended for all patients with heart failure.
Salt restriction
Salt retention with consequent oedema is a feature of heart failure. A low salt diet should be advised. Although no specific guidelines exist, excessive intake of salt should be avoided. Leaflets are available from the Irish Heart Foundation website outlining salt content of foods.
Weight monitoring
Patients should weigh themselves on a regular basis to monitor weight change, preferably as part of a regular daily routine. In the case of a sudden unexpected weight gain of > 2kg in three days, patients may increase their diuretic dose and should alert the healthcare team.
Immunisations
Pneumococcal vaccination and annual influenza vaccination should be considered in patients with symptomatic HF without known contraindications.
Medications
Diuretics
Diuretics reduce congestion in heart failure. They improve symptoms and reduce dyspnoea, ankle and pulmonary oedema. Loop diuretics, such as frusemide and bumetanide, are most commonly used. Diuretics can be used as a flexible dose regime in those with heart failure. At time of fluid overload, diuretics may need to be increased and at other times can be decreased or even stopped in some patients.
It is important to monitor patients for over-diuresis, eg. postural drop in blood pressure, rising urea and to consider reducing diuretic dose in these patients. Some patients may be educated to increase and decrease the dose of diuretic themselves in response to symptom and weight changes.
Thiazide diuretics can precipitate a large diuresis if used concurrently with loop diuretics and may be useful in some instances in the management of decompensation of heart failure (see ‘useful resources’ section at end of article).
Heart failure with preserved ejection fraction
Direct evidence to support a specific drug regimen to treat heart failure with a preserved ejection fraction (HFPEF) is lacking. Fifty per cent of patients with heart failure in the community have a normal ejection fraction.
The routine use of medications such as ACE inhibitors and beta blockers and the target doses noted above has not conclusively been shown to be beneficial in this patient group. However, these medications may be used to control other factors such as hypertension or ischaemic heart disease in patients with HFPEF.
Strategies that are currently recommended in the management of HFPEF include:
- Control of systolic and diastolic hypertension
- Control of ventricular rate in patients with atrial fibrillation
- Control of pulmonary congestion and peripheral oedema with diuretics
- Treatment of myocardial ischaemia.
Heart failure with low ejection fraction (LVSD)
Most clinical trials have focused on patients with a low ejection fraction. There is a strong evidence base for the use of ACE inhibitors and beta blockers in patients with a low ejection fraction in improving ventricular function, reducing mortality, reducing hospital admissions and improving patient wellbeing.
A meta-analysis showed that patients on ACE inhibitors9 had a lower total mortality (23% vs 27% for placebo, odds ratio 0.80, 95% CI 0.74-0.87) and a lower rate of readmission for HF (14% vs 19%, odds ratio 0.67, 95% CI 0.61-0.74).
A meta-analysis looking at benefits of beta blockers in patients with heart failure with reduced LV function showed that beta blockers significantly reduced total mortality at one year (odds ratio 0.65, 95% CI 0.53-0.80) and two years (odds ratio 0.72, 95% CI 0.61-0.84).10
Beta blockers also reduced hospitalisation for HF (odds ratio 0.64, 95% CI 0.53-0.79).
ACE inhibitors
Once diuresis has been achieved and the patient is at a stable weight it is common practice to start an ACE inhibitor first. The dose can be increased every two weeks until target dose is achieved. Target doses for individual ACE inhibitors are found in the ESC guidelines.
Beta blockers
A beta blocker should be used in all patients with heart failure and LVSD unless contraindicated or not tolerated. COPD is not a contraindication to beta blocker use and use of cardioselective beta blockers is recommended.
Newer and other therapies
A potential new direction for heart failure therapy for which evidence of benefit is emerging is ivabradine, a heart rate-lowering agent. Detailed discussion of other therapies such as digoxin, aldosterone antagonists and device therapies is outside the scope of this article. However, further details can be obtained from the ESC guidelines on heart failure.
Prescribing hints
Given the age group and comorbidities found in heart failure due to LVSD it is not uncommon for problems to arise in the use of medications in heart failure. A general guide to some of these problems is outlined below.11
- Be aware of over-diuresis – the patient may not require as high a dose of diuretic once medications such as ACE inhibitors and beta blockers are started. Aim for the lowest dose of diuretic to reduce oedema.
- Be aware of over-medication – certain medications may not add any benefit in heart failure, eg. calcium channel blockers, alpha blockers, and these may be stopped if issues such as hypotension are stopping titration of medications and there are no other compelling indictions for these medications
- Be aware of medications that may exacerbate heart failure.
Medication side-effects
Hypotension
If hypotension is asymptomatic it may not be necessary to change therapy. However, it is important to determine if there are any medications that can be reduced or stopped without affecting heart failure therapy, eg. calcium channel blocker, nitrates or vasodilators unless necessary for other conditions.
The dose of diuretic may also be reduced if no signs of oedema while monitoring for symptoms and signs of fluid re-accumulation. If symptoms persist it may be necessary to reduce the ACE inhibitor and/or beta blocker.
Ace inhibitors
Cough
Cough occurs predominantly with ACE inhibitors and occurs in 5-20% of patients.12 It is important to remember that cough may be due to uncontrolled heart failure or other illnesses such as COPD. If the cough is possibly due to heart failure it can be worth increasing the diuretic temporarily to determine if the cough improves. If the cough is suspected to be due to ACE inhibitor and is not causing distress the ACE inhibitor can be continued. If cough is distressing, an angiotensin receptor blocker should be substituted. Cough normally resolves within two weeks of stopping the drug but can take up to four weeks.13
Increasing creatinine
Some increase in creatinine is expected during use of ACE inhibitors due to the decline in GFR. Particular care must be taken in those with an elevated creatinine already who may require specialist supervision. A rise of up to 30% from baseline is acceptable in those with normal creatinine. If rise is greater than 30% review all medications for those which may cause nephrotoxicity, eg. NSAID, and determine if dehydrated due to over diuresis.
Hyperkalaemia
This occurs in 3.3% of patients on ACE inhibitors.14 Difficulties in transport of samples in general practice may mean that accurate estimation of potassium levels may be difficult in some areas. Mild elevations in potassium may be tolerated (< 5.5mmol/l).
It is important to determine if other potassium-sparing agents such as amiloride are being used. More marked elevation may require cessation of therapy with ACE inhibitor or referral to the emergency department.
Angio-oedema
This may occur anytime during the use of ACE inhibitors and requires termination of treatment with them.
Beta blockers
Bradycardia
Low heart rate is the main factor that limits titration of beta blocker doses.15 If the heart rate is less than 50 beats per minute and symptoms of heart failure are worsening the dose of the beta blocker should be halved.
It is important to review the need for other drugs which may be slowing the heart rate also, such as digoxin and verapamil. An ECG to determine if heart block is present should be performed.
Worsening symptoms
Patients may have a period of worsening of HF symptoms when initiating beta blockers. This is minimised by starting at extremely low doses and titrating up every two weeks until target doses are reached.
The diuretic dose can be increased by 50% to alleviate oedema if present. If heart failure symptoms persist the dose of beta blocker may be reduced.
Medications to avoid in heart failure
Patients with heart failure are predominantly elderly and have multiple comorbidities. Therefore, polypharmacy and drug interactions and adverse effects are common in this patient group.
The STOPP and START criteria have been used to identify potentially inappropriate medications and highlight prescribing omissions in elderly patients.16
Some potentially inappropriate medicines for use in patients with heart failure are listed below:
- NSAIDs are associated with an increased risk of HF exacerbation and impairment of responses to ACE1 and diuretics
- Negatively inotropic calcium channel blockers in heart failure with left ventricular systolic dysfunction (nifedipine, verapamil, diltiazem) can precipitate heart failure exacerbation. Amlodipine and felodipine are preferred
- Pioglitazone can cause fluid retention which may precipitate heart failure
- Testosterone can also cause fluid retention
- Pregabalin has been associated with exacerbation of heart failure in elderly patients.17
Conclusion
Heart failure is an important condition with significant impact on patients, their carers and the healthcare system.
An accurate diagnosis is vital to planning the management of heart failure and the use of appropriate medications can help reduce hospital admissions and mortality and improve quality of life for patients.
 (click to enlarge)
(click to enlarge)
