OBSTETRICS/GYNAECOLOGY
Primary ovarian ectopic pregnancy
Recognition of an ovarian ectopic pregnancy is of critical importance and should be considered in the differential diagnosis of acute abdominal pain in women of reproductive age
December 1, 2022
-
Primary ovarian ectopic pregnancy is one of the rarest forms of ectopic pregnancy. Its incidence after natural conception ranges from one in 2,000 to one in 60,000 deliveries and accounts for 3% of all ectopic pregnancies.1 It is estimated that ovarian pregnancy occurs in one in 25,000-40,000 pregnancies.2 It develops in approximately 0.5-3% of all ectopic gestations. The specific cause of ovarian pregnancy is unknown but there appears to be a link to the use of an intrauterine device (IUD).3
We present a case where a 19-year-old woman (P1+0), was diagnosed with ovarian ectopic pregnancy (OEP) and was confirmed as primary ovarian ectopic pregnancy both intraoperatively and histopathological, and managed with laparoscopic excision of ectopic pregnancy.Diagnosis
Diagnosis of primary ovarian ectopic pregnancy is made in asymptomatic pregnant women by obstetric ultrasonography. Histological surgical diagnosis is made using Spiegelberg’s criteria,4 which includes:
- Gestational sac located in the region of ovary
- Ectopic pregnancy is attached to the uterus by ovarian ligament
- Ovarian tissue in the wall of gestational sac
- Fallopian tube on the affected side is intact.
Case report
A 19-year-old woman (P1+0), presented and was admitted to hospital at six weeks gestation with two days history of per vaginal spotting and no abdominal pains. Patient had no significant past surgical and medical history. She had a regular menstrual cycle of four days in a 28-day cycle. She had one living child, childbirth was 18 months previously via normal vaginal delivery.
On presentation, she was vitally stable with blood pressure of 110/70. There was no tenderness, guarding and rigidity on abdominal examination. On per vaginum examination, no cervical motion tenderness was noted, with normal anteverted uterus. Urine pregnancy test was positive and beta hCG was 1,202 IU/L. Repeated levels of beta hCG were 1,355 IU/L and 1,898 IU/L. The patient initially declined any surgical intervention and opted for expectant management.
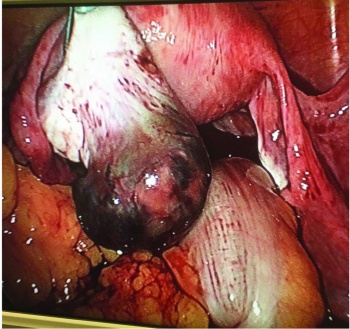
A day after the third level of beta hCG, the patient began complaining of severe lower abdominal pains and became hypotensive with blood pressure 80/45. A laparoscopy was performed due to severe pain and hypotension. Ectopic pregnancy was identified over the left ovary. Uterus, bilateral fallopian and right ovary were normal. There was pelvic haemoperitoneum and no signs of adhesions or Fitz-Hugh-Curtis syndrome (FHCS). Laparoscopic removal of left ovarian ectopic pregnancy was performed by diathermy scissors.
Postoperative period was uneventful and the patient conceived seven months later and delivered normally a full term baby. Histopathological examination of ectopic mass showed left ovarian ectopic pregnancy. (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)