CHILD HEALTH
Administering intramuscular and subcutaneous injections in children
Sound clinical judgement and individualised assessment are essential to ensure safe practice when administering injections to children
October 1, 2012
-
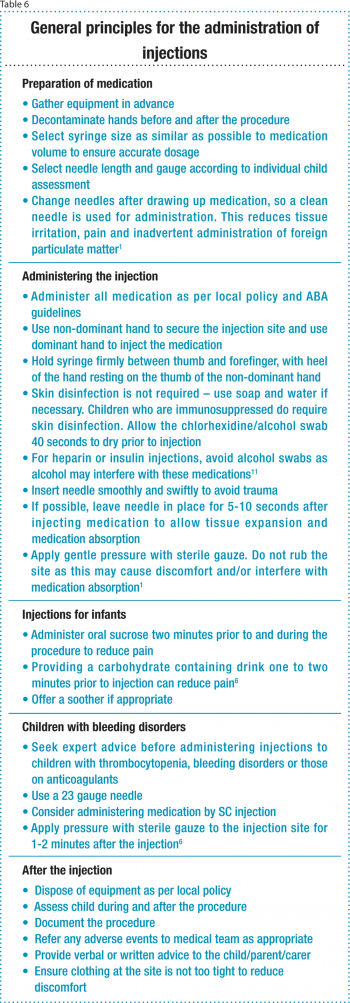
Children and nurses often view the administration of injections as a traumatic procedure. Nurses aim to avoid administering injections to children unnecessarily. However, certain medications may only be administered by injection, as alternative routes are not viable or may not facilitate absorption.1 Correct injection technique can reduce complications, injury and discomfort for the child.
Recent years have seen a reduction in the use of intramuscular injections in particular. The introduction of alternative analgesia techniques, such as epidurals, intravenous infusions, and patient and nurse controlled analgesia has reduced the volume of injections administered. Despite this, the administration of injections remains a fundamental nursing practice and children’s nurses need to update their knowledge and skills.
Necessary skills for good injection technique include knowledge of: anatomy and physiology; pharmacology; suitable injection sites and injection techniques for children; clinical holding; and effective communication skills.
Evidence-based nursing guidelines for the administration of both intramuscular (IM) and subcutaneous (SC) injections were created within Our Lady’s Children’s Hospital to support best practice and safe administration of medication.
Individual child assessment
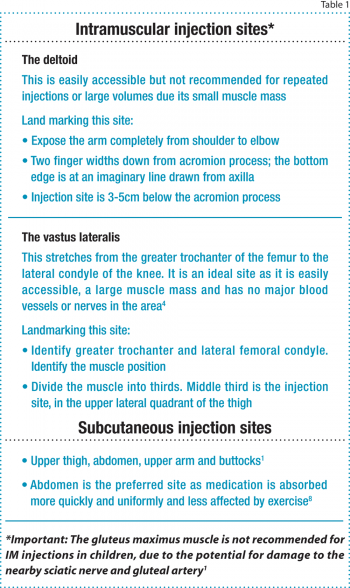
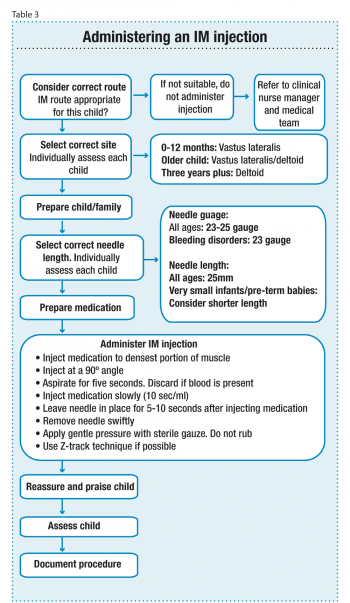
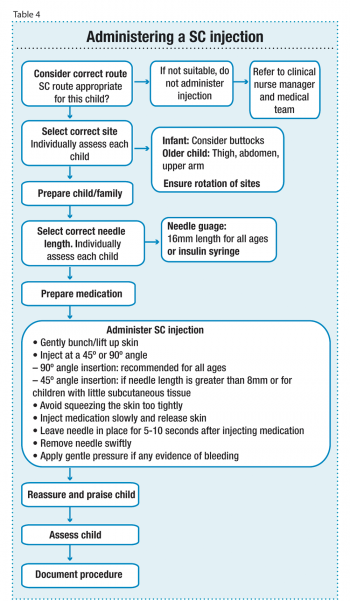
The nurse should initially assess whether an injection is the optimum route for the child. There is no universal agreement on optimum injection site, needle size or injectable volumes, therefore, children’s nurses must recognise the importance of individual child assessment and clinical judgement to ensure best practice when administering IM and SC injections to children (see Table 1).

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)