WOMEN’S HEALTH
The four ‘Rs’ in dealing with domestic violence
In dealing with domestic violence the most important thing is to listen and then offer help
April 9, 2014
-
Domestic violence is common, serious and frequently not identified. It can occur in any intimate relationship and can be physical, sexual and/or psychological. Both women and men experience violence. However, the prevalence of more serious abuse is far higher for women. The Irish National Study on Domestic Abuse 2005 reported that 15% of women and 6% of men had experienced severe abuse. This study also reports that women are twice as likely to experience severe physical abuse, seven times more likely to experience sexual abuse and three times more likely to experience severe emotional abuse than men. For the majority of victims, violence is endured as a chronic long-term condition that escalates over time.
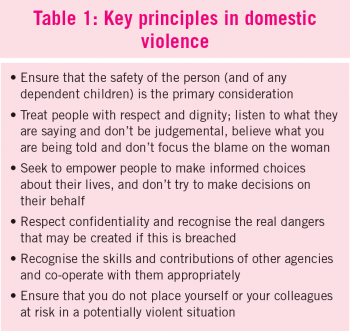
Domestic violence may result in physical injury, chronic physical ill health and/or emotional and mental health difficulties. It may result in death. Women are more likely to disclose violence to their GPs than to any other professional group. Therefore, the initial response of the GP is of profound importance (see Table 1).
In dealing with domestic violence, the most important role of the GP or practice nurse is to listen and then offer help. The aim is not to fix the problem but to acknowledge the issue, inform the victim about options and support their decisions. The approach to dealing with domestic violence can be summarised as follows:
- Recognise: Know the signs, indications and sequelae of abuse
- Respond and record: Know how to deal with the issue of abuse
- Refer: Make a good, appropriate referral
- Review: Ensure that the patient is encouraged to return for follow-up.
Recognise
Women are not likely to disclose domestic violence, particularly in the early stages. The strongest determinant of disclosure is clinician inquiry. Those who are not ready to disclose may present with injuries inconsistent with explanations, frequent presentations with chronic medical/psychological problems or ‘by proxy’ with a child with frequent minor complaints. Women who present as victims of choking or attempted strangulation warrant special attention as these injuries are ‘red flag’ indicators of a high risk abusive situation.
The greatest risk factor is being female. Domestic violence can begin or escalate in pregnancy. A woman is most at risk when she decides to leave a violent relationship. Other vulnerable groups include women with mental health problems, traveller women, women from migrant communities and those with disabilities.
Children are affected by domestic violence. They may be victims, witnesses or forced to participate. Where a risk to children is identified, immediate action must be taken. Current child protection guidelines are discussed in the full ICGP guideline on domestic violence (see www.icgp.ie/QIPdomesticviolence).
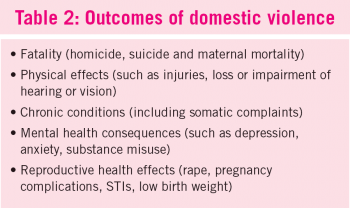
The outcomes of domestic violence impose a substantial burden on health and social services. Domestic violence may result in, or contribute to, a range of outcomes (see Table 2). The outcomes of domestic violence in terms of physical and psychological injuries tend to be considerably more negative for women victims than for men victims.
Respond
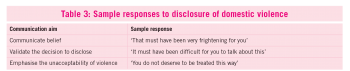
Once a disclosure is made, it is important to listen and respond according to the general principles outlined in Table 1. It may be helpful to consider how one would respond to disclosure (see Table 3).
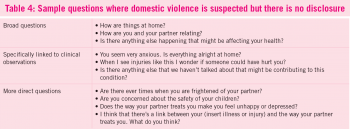
Where you suspect domestic violence but there is no disclosure, questions may initially be broad in focus or may be linked to specific clinical observations (see Table 4). Do not ask a patient about violence unless the patient is alone and you cannot be overheard.
Record
Confidentiality is particularly important in general practice where other family members, including the perpetrator, may also be patients of the practice. Contemporaneous medical records documenting injuries/incidents are helpful if legal action is subsequently taken.
It is helpful to record specific details of the incident as reported. Injuries may be documented on a body map. Samples are provided in the full guideline on domestic violence.
Refer
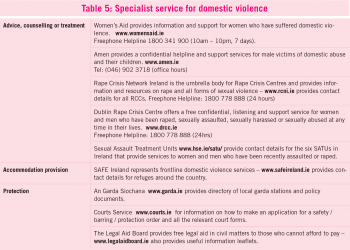
Referral, in the context of victims of domestic violence, is different from the standard referral process familiar to GPs. The approach when such a disclosure is made should be to empower the patient to undertake action that she deems appropriate at a time that she deems appropriate. It is helpful to signpost appropriate specialist services (see Table 5).
Accessibility of services varies depending on your location and it is important for you to familiarise yourself with local services, particularly when you move into a new practice. www.cosc.ie provides publications and links to services.
Referral to another individual or agency should have the approval or express consent of the patient as ‘referral’ by the GP to an agency or An Garda Síochána without the patient’s direct involvement is rarely helpful and potentially harmful. It is often advisable to encourage your patient to make the contact herself. This may take the form of a telephone call in the privacy of your consulting room with your encouragement.
Review
Where a GP or practice nurse suspects domestic violence but there is no disclosure, it is important to keep the door open and signal willingness to help at any stage in the future.
Dealing with victims of domestic violence can be frustrating. It is important that GPs and practice nurses recognise their own limitations, have support structures in place for themselves and ensure the safety of themselves and their practice staff.
New ICGP guideline
The ICGP provided a clinical guideline on the topic of domestic violence in 2008 and the updated second edition is now available on www.icgp.ie/QIPdomesticviolence and will be launched at the AGM this year. The guideline supports GPs in improving the quality of care for those who have experienced domestic violence, provides advice on how to ask a patient about violence, how to respond to disclosures and signposts appropriate supports.
Acknowledgement
The authors acknowledge the funding for the ICGP guideline by Cosc, The National Office for the Prevention of Domestic, Sexual and Gender-based Violence and the contribution of the Advisory Group.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)