DIABETES
ENDOCRINOLOGY
Focusing on feet
Ronan Canavan, clinical lead on the national diabetes programme, gave an update on the 2011 foot care model and its outcomes to date
December 15, 2014
-
The first Irish model of care for the diabetic foot was set up in November 2011. Building on international experience and knowledge around the diabetic foot, the theme of the programme was to direct targeted foot care towards those most at risk based on proper screening of cases.
Dr Ronan Canavan, consultant endocrinologist and clinical lead on the National Diabetes Programme, presented the model of footcare for Ireland to date, how implementation of the programme has turned out and what the outcomes are so far, at the recent Inaugural Conference of the National Clinical Programme for Diabetes in Farmleigh, Dublin.
Dr Canavan mentioned an Irish endocrinologist’s expression about diabetic footcare and how ‘it’s not rocket science, it’s much more complicated’.
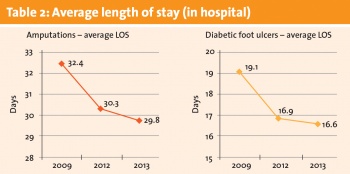
“What he means is that despite that the management of the diabetic foot is based on a lot of simple principles, well working models and lots of understanding about how patients get the worst outcome in terms of amputations and diabetic foot ulcer, the outcome still proves resolutely difficult to get in terms of reducing amputations and diabetic foot ulcers.”
Dr Canavan outlined the background to the current Irish model of footcare by focusing on two studies1,2 from the US and Germany. He also emphasised how history has shown that ‘one shot’ at improving diabetes foot care won’t do it.
“You have to go back, refocus and revisit. You have to keep up with the data and if you’re not making any real change [in improving diabetic foot outcome] you have to go back and see if there is any fresh evidence and see if there’s anything else that can be done,” explained Dr Canavan.
This was the case with the diabetic foot care programme set up in Germany in the mid-90s, which showed that after years of foot care programme implementation, there was no real impact on outcome, and so the programme was analysed and changed. Subsequent reviews of outcomes showed that they improved compared to before intervention.
“A simple fact is that 80% of diabetic foot amputations are preceded by a foot ulcer,” highlighted Dr Canavan.
He used the Pecoraro model3 to illustrate how amputations are preceded by a line of events starting at diabetic neuropathy; the build-up of hard callus; leading to a foot ulcer, which may get infected; and if this infection fails to heal, that’s when the amputation may occur.
“With this simple fact on board, we can build up a model of where to direct specific intervention to try and cut off the pathway to amputation,” he added.
The Irish model of foot care
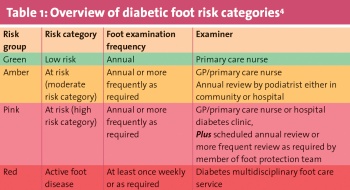
Basically, the idea of the 2011 model of care for the diabetic foot was to target foot care towards those most at risk based on proper risk stratification and triage.
“The model of care was introduced in 2010 at a time when things were getting bad, resources were being squeezed and any resources available had to be used for very cost-effective intervention.
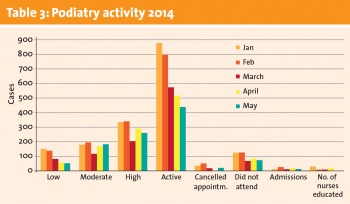
“So limited resources, around a million euros, was directed towards employing 16 podiatry posts within hospitals to set up a foot protection team to feed into the diabetes multidisciplinary foot care teams,” said Dr Canavan.
But by mid-2013, less than half of these HSE podiatry posts had been filled, Dr Canavan added. However, by the time he presented at the Farmleigh conference, he was able to give slightly more positive news in that all 16 positions have now been filled.
Outcomes to date
“The real change that the model has brought on in Ireland for the standard approach to the diabetic foot, is where it lies in terms of risk stratification,” said Dr Canavan.
“Basically what this means is that people at the lowest risk rarely go on to amputation,” he added.
Dr Canavan further explained that this allows for resources to be put in where they are most needed, so that patients in the low risk category get screened annually to make sure they stay in that category, while the patients in the high risk category get intensive treatment by a multidisciplinary foot care team.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)