CARDIOLOGY AND VASCULAR
Heart failure success story
A 'virtual consult' heart failure initiative has led to quicker access to specialist opinion and a reduction in outpatient referrals and hospitalisations
May 27, 2016
-
Heart Failure is a growing problem in Ireland and currently affects 90,000 people; it predominantly affects the elderly population who often find it difficult to access hospital services due to social circumstances.
Morbidity and mortality is high, with heart failure being one of the most frequent causes of hospitalisation. It is estimated that in 2012 heart failure cost almost €660 million in the Republic of Ireland. Almost 50% of direct costs related to patients being hospitalised and 7% of all hospital inpatient beds were taken up by patients with heart failure. The total annual bed days taken up by heart failure patients is over 231,000 days.
GP survey on heart failure
A recent national survey of GPs demonstrated that 90% of GPs felt that waiting times for outpatient appointments were a major barrier to heart failure care and 38% of GPs stated that patients being unable to travel to outpatient appointments is a major barrier to heart failure care.1
Often, emergency hospitalisation takes place to try and deal with emerging issues in people with heart failure in the absence of another effective and efficient means of dealing with the situation.
Many of the reasons for outpatient referral can be appropriately dealt with initially through modern communication technologies such as web-based conferencing. Other services such as Project ECHO have implemented this strategy for conditions such as hepatitis C and demonstrated similar outcomes for patients managed in primary care with specialist online support compared to those managed in a university hospital.
A randomised controlled trial in the UK2 showed that virtual outreach consultations across a number of specialities resulted in significantly higher levels of patient satisfaction compared to standard outpatient appointments and led to substantial reductions in numbers of tests and investigations.
The Heartbeat Trust
The Heartbeat Trust is a charity organisation registered in Ireland which seeks to lead the way in the prevention and treatment of heart failure as well as discover and develop new therapies for this complex and varied condition.
Patient services are provided via the heart failure unit in St Michael’s and St Vincent’s hospitals in Dublin. St Michael’s is also home to the STOP-HF service aimed at prevention and early detection of heart failure.
Virtual consultation
Prof Ken McDonald, a cardiologist in St Vincent’s is medical director of the Heartbeat Trust and pioneered a virtual consultation service for local GPs.
The key to virtual consultation is prompt access to specialist opinion and diagnostics, resulting in a significant reduction in outpatient referrals and hospital admissions through improved communication between GPs and senior specialists.
Starting in mid-2014 and extending throughout 2015, the Heartbeat Trust ran a feasibility study in collaboration with local GPs on a virtual consultation service for the provision for online specialist advice direct to the GP as an alternative to outpatient referral in heart failure.
In this study, GPs could refer patients they had concerns or queries about to a virtual clinic. This was run by a consultant with a special interest in heart failure. The data from the referral was anonymised and transferred to a presentation template.
Between six to 10 practices logged into the consultation service each week. The consult session was (and is still) held at lunchtime. It began with a short educational presentation (five to 10 minutes) on a topic relevant to heart failure.
Following this, four to six cases were presented in an anonymised fashion by each patient’s GP where clinical questions were highlighted. This also served as an education resource for the other GPs who were online. Each case was discussed online and a consensus approach achieved for the further management of this patient’s condition.
Specialist tests were arranged directly if required without the need for specialist in-person review and results discussed on the virtual consult. Advice on medication changes or other strategies were also arranged. GPs can log on for just their case or for the whole meeting.
The virtual consultations are carried out using a system called Zoom, which allows interaction via telephone, desktop, laptop or an app on a smart phone.
Over the 18 months of the Virtual Consult Feasibility Study, the service received 282 referrals, of which 82% of patients did not require follow-on, face-to-face specialist review following the virtual consultation service. Over 50,000km in travel for the patient and their families was saved.
Successful approach
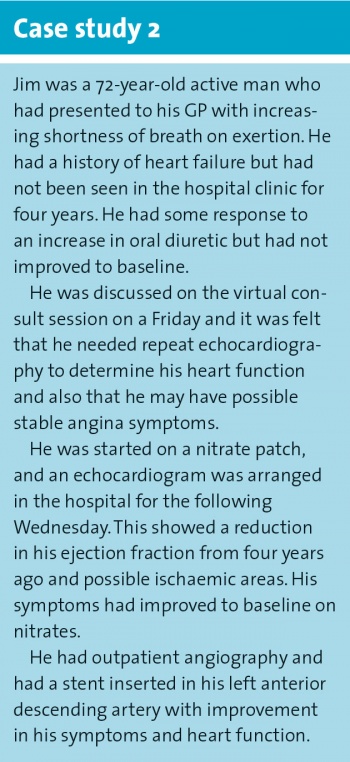
The success of this approach highlights its potential, particularly for this elderly patient group, and there have been a number of notable successes in avoiding hospital admission for the frail elderly and rapid access to diagnostics (see case studies 1 and 2) as well as providing a forum to discuss patients who may have complex needs or need rapid re-evaluation in the heart failure service.
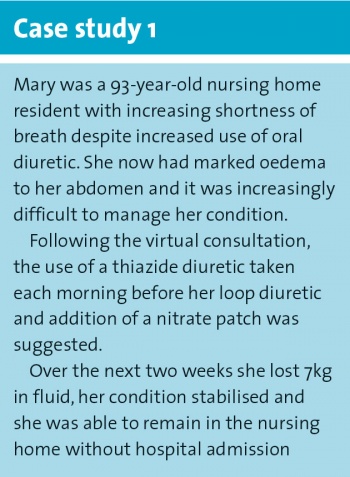 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)