RHEUMATOLOGY
Scleroderma: new milestones
Nurse specialists now play a key role in helping systemic sclerosis patients to cope with their illness
March 1, 2013
-
Systemic sclerosis (SSc) – more commonly known as scleroderma – is a rare, chronic, autoimmune connective tissue disease. Annual incidence in Ireland is estimated at 7-20 per million of the population, with a prevalence of 3-24 per million.
SSc has a largely female preponderance with reported female to male ratios 4:1.1 The average age of onset of disease is 50 years. It has a highly variable presentation and an unpredictable disease course.
An overproduction of collagen leads to skin thickening, a hallmark of the disease, and fibrosis of affected organs, including the gastrointestinal tract, lung, heart and kidneys.
Raynaud’s phenomenon is another universal manifestation of SSc.2 This is characterised by vasospasm in response to cold or other stimuli (eg. stress resulting in impaired perfusion of the distal extremities). In approximately 30% of patients, this can lead to digital ulceration.
SSc is associated with significant morbidity with cardiopulmonary complications, replacing renal crisis as being the most common underlying cause of mortality. The complexity and severity of SSc poses significant challenges to patients, physicians and multidisciplinary teams.
Appropriate management of SSc patients is complex. Issues such as early diagnosis of internal organ involvement and identification of those at risk of progressive disease come into play. Established predictors for increased mortality in SSc include: male gender; higher age at diagnosis; diffuse cutaneous SSc; and organ involvement.
Pathogenesis
The pathogenesis of SSc remains incompletely understood. It involves a complex interaction between the vascular and immune systems. Fibroblast cells also play a key role. Pathogenesis can be subdivided into an early inflammatory phase and a late, more fibrotic phase.
The pathogenic process is driven by a complex interplay between inflammatory cells, endothelium and fibroblast cells. The latter are key players in skin and organ fibrosis. As in various other rheumatologic conditions, the pathogenesis of SSc is partly based on genetic background and modulated by environmental factors.
Classification and diagnosis
As a result of the variety in disease presentation, SSc can be difficult to recognise properly and early in the disease process. Rheumatologists categorise patients into two well-recognised subsets depending on the degree of cutaneous involvement. The categories are: limited cutaneous SSc (lcSSc) and diffuse cutaneous (dcSSc).
The main difference between these two groups is that in lcSSc skin thickening is limited to the face and distal limbs, sparing the trunk. The limited type of SSc is more common amongst Caucasians.
A common subset of lcSSc is CREST: calcinosis, Raynaud’s phenomenon, oesophageal dysmotility, sclerodactyly, telangiectasia. This acronym was devised to outline the more common manifestations of lcSSc. Patients with a diagnosis of lcSSC have a significant late incidence of pulmonary hypertension (10-15%) in isolation or in combination with interstitial lung disease.3
In dcSSc, patients experience rapid onset of skin changes involving skin thickening of the proximal extremities (ie. upper arms and thighs), and sometimes the trunk. These symptoms may develop within one year after the onset of Raynaud’s phenomenon.
Visceral organ involvement is common and complications may include interstitial lung disease, pulmonary arterial hypertension, rectal cancer, gastrointestinal disease and myocardial dysfunction. These patients may also develop digital ulcers.
SSc and auto-antibodies
Auto-antibodies (ANAs) are one of the strongest predictors of disease course and outcome in SSc.4 ANAs are the hallmark of SSc and are detected in more than 95% of patients. The three most common individual SSc-related ANAs are: anti-centromere antibodies (ACA); anti-topoisomerase antibody (ATA); and anti-RNA polymerase 111 (ARA).
ACA antibodies are most frequent among Caucasians and rarely seen in black patients. There is a high prevalence of ACA in lcSSc. ACA positive patients carry a higher risk for the development of pulmonary arterial hypertension.5
There is a predominance of presence of ATS in dcSSc. Its presence is a strong predictor of the development of pulmonary fibrosis and digital ulceration. ARA positivity is strongly linked with dcSSc. This holds a high prediction for the development of scleroderma renal crisis.
Owing to the fact that a strong pattern exists between the type of antibody present and the pattern of organ complications and survival in SSc, antibody testing is essential in disease assessment.
A history of Raynaud’s phenomenon, ANA positivity, puffy fingers, disease-specific auto-antibodies and a scleroderma pattern on a nail fold capillaroscopy (a non-invasive test using a light and probe to view capillaries in the nail fold bed) are all indicative of a preclinical state.6
It is vital for early detection that health professionals in primary, secondary and tertiary care are aware of the early signs of SSc, and also of the appropriate action to take. Patients who are suspected of having SSc should be referred to a rheumatologist for confirmation of diagnosis.
Role of the nurse specialist in SSC
The nurse specialist has a key role in helping patients to cope with their illness. Symptoms can be debilitating, and range from digital ulcers to intestinal problems. A new position of national systemic sclerosis research nurse commenced in 2011 in Ireland. Patients referred to the SSc nurse receive a comprehensive physical and functional assessment.
The most important aspect of this nurse specialist’s role is one-to-one patient education. This covers various aspects of the illness such as the disease process, understanding and coping with symptoms, medication management and blood monitoring, wound management, and coping daily with a chronic illness.
The research aspect of the SSc research nurse specialist involves maintaining observational registries, and recruiting and monitoring for SSc clinical trials. A key aim is to capture all people living with SSc in Ireland. A national SSc registry is currently being established. This is a collaborative effort involving all participating rheumatology centres in the country with the ultimate aim of improving outcomes in this rare disease.
Ireland’s registry is being supported and part-funded by the Irish Raynaud’s and Scleroderma Society. It is the intention of key stakeholders involved in this project to enrol patients on both the Irish SSc registry and the European League Against Rheumatism (EULAR), with affiliated EULAR Scleroderma Trials and Research Registry (EUSTAR).
Linking all centres with EUSTAR will be beneficial in allowing centres in Ireland to collaborate in research efforts internationally. Furthermore, access to registry data will improve disease understanding and assist in standardising assessment and treatment across different centres.
Treatment
Although there is still no cure for SSc, studies on the pathogenesis of the disease are providing a growing number of molecular targets for potential therapeutic intervention. Treatment of SSc involves both non-pharmacological and pharmacological modalities. Therapy is directed at three compartments: the vascular system, the immune system and tissue fibrosis (see Table 1).
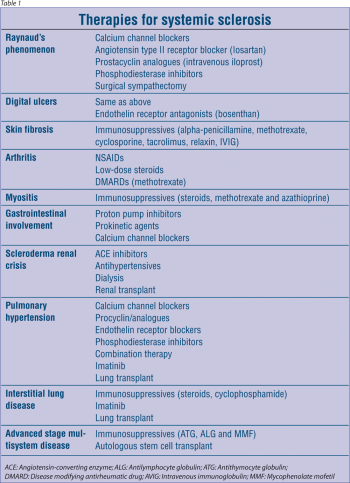 (click to enlarge)
(click to enlarge)
