RESPIRATORY
Management of people cocooning with COPD
COPD Support Ireland has warned that COPD patients may not be seeking medical attention due to fear of contracting Covid-19 in hospital
June 9, 2020
-
COPD admissions through emergency departments normally account for a significant proportion of presentations; however, concern has been raised that people with chronic obstructive pulmonary disease (COPD) are delaying seeking medical help if they have a flare-up in symptoms due to fears of contracting Covid-19 in hospital.
Prof JJ Gilmartin, consultant respiratory physician and chair of COPD Support Ireland, warned that such delays could result in a more severe exacerbation that may ultimately lead to pneumonia, prolonged oxygen therapy or even the need for ventilatory support.
The estimated 500,000 people in Ireland living with COPD make up one of the vulnerable groups more at risk of serious illness if they contract Covid-19. Prof Gilmartin has urged patients not to put their health in danger and has sought to reassure them that hospitals are taking every precaution to ensure their maximum health protection.
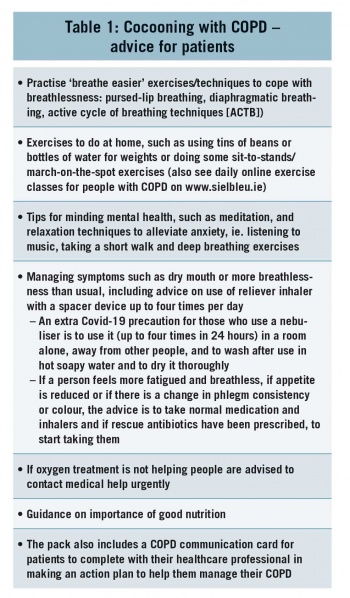
His comments came at the launch of a ‘Cocooning with COPD’ information pack with tips and advice for protecting physical and mental wellbeing for people with COPD. The pack contains a COPD & Me self-management booklet, the ‘Staying well – cocooning from coronavirus’ booklet, and a COPD communication card, and was developed in conjunction with the HSE National Clinical Programme and the COPD advice line. This pack is available to download at www.copd.ie or can be ordered for postal delivery free of charge by texting ‘COPD’, plus name and address to 51444 (standard call).
According to the most recent statistics, there were 40,444 admissions to hospitals nationwide as a result of COPD between 2016 and 2018. Indeed, COPD is the most common disease-specific cause of emergency hospital admission among adults, with Ireland having the highest hospitalisation rate for COPD of all OECD countries in 2015, the last year for which international data is available.1
People who have questions about how best to manage COPD, and who wish to speak to a specialist respiratory nurse for information and advice, can telephone the national COPD Adviceline on Freefone 1800 83 21 46 (a call-back service open 9am to 5pm on weekdays).
Prof Gilmartin urged patients to speak to their GP or COPD hospital outreach team if their COPD worsens. “For good public health reasons right now, physicians are not in a position, at least initially, to see patients in person for routine check-ups, and instead are having to rely on more limited phone and video consultations. However, we are anxious that early signs of a disease flare-up might not be immediately apparent through these virtual clinics. We are also concerned that many people with COPD who are having a worsening of symptoms are really afraid to come to hospital and are staying at home for fear of contracting Covid-19.
‘I would strongly urge people with COPD to pay close attention to their own signs and symptoms. They will know if they are having a flare-up of COPD and, if concerned, they should speak to their GP or COPD hospital outreach team without delay so that they can be monitored.
“Patients should know that hospitals have different entry pathways for Covid and non-Covid patients and that every possible precaution is being taken to remove any risk to them. To be honest, there is a greater risk to their health by not attending hospital, or holding out on coming until they can no longer cope. Leaving things until the last minute could result in a more severe exacerbation that may ultimately lead to pneumonia, and prolonged oxygen therapy or even ventilatory support. This can be avoided but we need people to take action promptly.
“In addition, the National Clinical Programme is actively engaged in developing platforms for virtual/remote clinics and virtual rehabilitation programmes to augment the current measures aimed at minimising any risk for COPD patients. There is an ever-expanding menu of healthcare delivery methods available, and your GP or COPD outreach team will endeavour to tailor this to best suit you at this time.”
The ‘Cocooning with COPD’ information pack features information on COPD, its risk factors, symptoms and diagnosis. It also provides easy-to-understand advice on self-care for patients (see Table 1).
 (click to enlarge)
(click to enlarge)
