DIABETES
Organise to achieve
For patients, well organised, co-ordinated and delivered care can be the difference between having diabetes and suffering from diabetes
December 15, 2014
-
With the appropriate supports, GPs and practice nurses can successfully manage type 2 diabetes entirely in a community setting, this was according to Prof Colin Bradley, head of the department of general practice at UCC, who was speaking at the on ‘Managing diabetes in the Irish primary care setting – lessons for the future of chronic disease management’ at the Inaugural Conference of the National Clinical Programme for Diabetes at Farmleigh, Dublin.
Prof Bradley introduced himself as a GP who was expert in people who have diseases, rather than an expert in diabetes, a researcher but not a diabetes researcher and a teacher who does not teach people how to treat diabetes.
He also said that he had an important message for those attending the conference: GPs in Ireland are disillusioned with diabetes care programmes and are seeking a re-engagement.
“I’m not here on behalf of any particular group of general practitioners, but I am immersed in that world and many of my colleagues are very keen for me to tell you how discomforted, disillusioned, disrespected and disregarded we feel in relation to the diabetes programme.”
Prof Bradley stressed that he hoped that this was a temporary difficulty that could be overcome by a re-engagement by the Diabetes Care Programme with GPs and that though some 'feisty discussions' that a more constructive situation could be achieved.
Setting up the DIG
Drawing a line under this message, Prof Bradley went on to give an overview of the Diabetes Interest Group (DIG). The Group arose from a Heartwatch funded course on diabetes care that was run by UCC in 2001 for GPs and practice nurses. During the course, participants recognised deficiencies in the care of their own patients. This led to the establishment of the DIG (subsequently renamed as Diabetes in General Practice DIGP) with the aim of improving the care of those with diabetes from within general practice.
“Out of that course there came an awareness among my colleagues that certain significant deficiencies of care existed around our own patients with diabetes. There was also an awareness that there was never going to be a complete secondary care solution to the problem. There was a recognition that such was the extent of the problem, and such was the range of problems that this group had that it was never going to be solved by a hospital-only approach so we looked at what we could do at our own level to improve the care of this group in general practice.”
The philosophy of the group was based around peer education and trust, the use of audit and subsequent data, collegiality and commitment to quality improvement.
The peer education is based around three to four small, CME-type groups of 10 to 12 GPs with presentations on specific topics and case presentations which are internally resourced and led by GPs for GPs. Prof Bradley described these discussion-based groups as a 'powerful learning tool'.
GPs sought more education in this area and in response a university-level diabetes module was developed that involved additional external resources for source materials and tools such as blended and distance learning as well as ongoing peer learning.
Prof Bradley stressed that audit was key to the success of the DIG and completion of regular audit was a key commitment for membership of the group. This included the prerequisite that, following the Scottish exemplar, each practice must establish a diabetes register and the collection of a common agreed set of data in relation to patients with diabetes.
According to Prof Bradley, this enabled an insight into what was happening in the area of diabetes generally as well as how each practice was doing comparatively. The data that is collected is then collated and compared, with analysis assisted by a clinical academic and statistician.
Current situation
From an initial group of 10 practices, the DIGP now has 46 enrolled – with a waiting list for more to get involved – that are currently monitoring more than 5,700 patients. The Group continues to hold regular educational meetings and has increased the scope of audits. The annual conference attracts more than 250 delegates each year.
The DIGP is also working in a collaborative role on important projects such as the Diabetes Register study, funded by the HRB, and the Retinopathy Screening Project, in collaboration with the HSE.
The DIGP also has a community-based diabetes nurse specialist – funded through charitable donations and continues to be involved with the Diabetes in Primary Care module in UCC as mentioned above.
Latest audit results
In terms of process of care audit outcomes, according to Prof Bradley, the DIGP results are ‘pretty good’: Of patients with type 2 diabetes, some 90% (2,245) achieved a blood pressure reading within desired levels, 86% (2,143) for HbA1c readings, 89% (2,205) for cholesterol, 40% for albumin creatinine ratio (ACR), 60% for smoking status and 49% for BMI.
Among patients with pre-diabetic conditions figures were 86% (264) from blood pressure control, 89% for cholesterol, 68% for smoking status and 33% for BMI.
Prof Bradley described BMI as the 'missing link' that they were struggling to 'get hold of' but stated that this was a 'pinch point' for other diabetes programmes, both nationally and internationally.
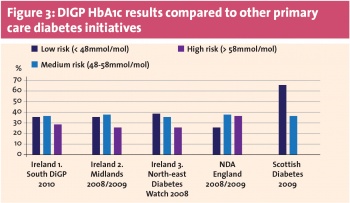
Looking at the latest audit results in relation to outcomes, Prof Bradley said that in patients with type 2 diabetes 37% (826) had achieved target blood pressures, 36% (764) had achieved glycaemic control of under 6.5% (48mmol/mol) and 58% (1,235) of under 7% (53mmol/mol). Some 65% (1,425) reached the cholesterol targets, with 68% (1,244) meeting triglyceride targets.
In patients with pre-diabetic conditions 28% (27) had achieved target blood pressures, 47% (75) reached the cholesterol targets, with 77% (176) reaching triglyceride targets.
“Again, it is a mixed picture. We’ve made some headway with glycaemic control and done pretty well in relation to cholesterol but getting blood pressure to target remains a challenge,” said Prof Bradley.
He went on to suggest that perhaps the targets themselves needed to be revisited but said this would be a discussion for another day.
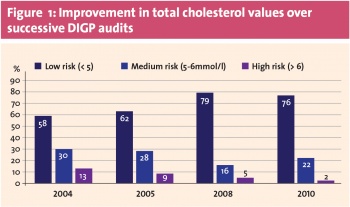
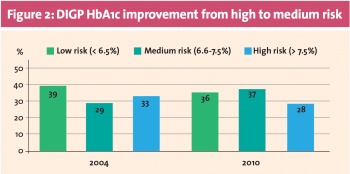
Looking at DIGP audit results (Figures 1 and 2), he said that the figures showed that we face a very similar challenge in relation to the those with diabetes and those in the pre-diabetes groups.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)