MENTAL HEALTH
The Mental Health Act – training shortcomings
Many GP trainees feel that their training does not provide sufficient education regarding the Mental Health Act
April 28, 2016
-
Approximately 44% of the Irish population experience mental health problems either personally or through their family or friends. The former Mental Health Act (MHA) legislation dated back to 1945 and was subject to major modification and improvement in Ireland in 2001. The purpose of the MHA is to protect those who are admitted involuntarily and to monitor and maintain the best standards of care and treatment in our mental health services, which are regulated by the Mental Health Commission. The MHA is an involuntary admission process for adults and children. The usage of the Mental Health Act is well known to be a difficult and challenging aspect of primary care.
The MHA is used where because of mental illness, disability or dementia, a person is likely to harm themselves or others, or due to the severity of the illness, their judgement is so impaired that failure to admit them to an approved centre may lead to a deterioration of their condition. Additionally, this can be used when the detention and treatment of the person would likely benefit and alleviate their condition to a material extent.
The exclusion criteria for an involuntary admission to an approved centre includes when a person is suffering solely from a personality disorder, is socially deviant or addicted to drugs or intoxicants.1
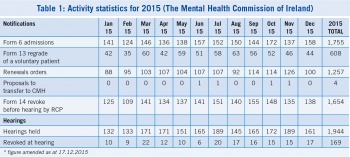
According to the Mental Health Commission 1,755 patients were admitted under the Mental Health Act, via form 6 involuntary admissions in 2015.3
Current practice
The current practice of the MHA involves GPs to a great extent. The GP has the first contact of the application from the person acting on behalf of the ill patient. This application can be made by a spouse or relative, an authorised officer, a member of An Garda Síochana or any other person who has not been disqualified by the law.4
The GP’s role is firstly to assess and examine the patient regarding suitability for detention under the MHA.5 The GP needs to make specific considerations and must fulfil the need, and the right to respect the dignity, autonomy, integrity and privacy of the patient.
A study by Jabbar et al which was published in 20116 found that 62.9% of GPs felt that the MHA was not user- friendly, and 85% of GPs reported an increased workload and 53% reported other difficulties. Additionally, they found that GPs who had received training about the legislation found it more user friendly.
Audit
The aim of this study was to discover GP trainees’ perception about their knowledge and training relating to the Mental Health Act. All north-east GP trainees were asked to answer 10 questions relating to their knowledge and perceptions of their training in the use of the Mental Health Act.
Methods
An anonymous 10 point questionnaire was created online by a GP trainee (SHO in psychiatry). The North-East GP Trainee Scheme administrator was contacted and agreed to send the questionnaire to all north-east GP trainees. The completed questionnaire results were kept anonymous.
Results
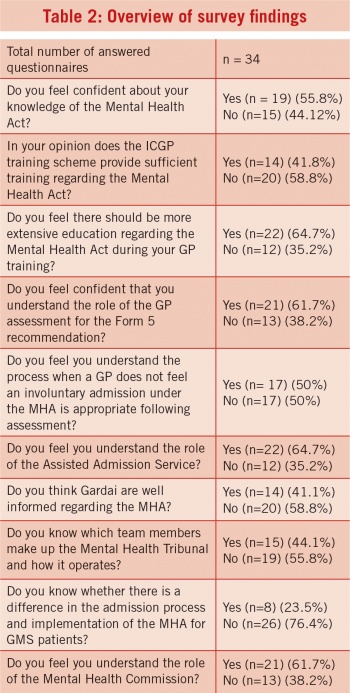
The number who responded to the questionnaire was 34 out of 58 trainees. This represented a 58.6% uptake.
Of those who replied, 55.8% of North East GP trainees felt confident about their knowledge of the MHA, while 61.7% felt confident that they understood the role of a GP assessment during a form 5 recommendation.
However, 58.8% of trainees felt that their training scheme was not providing sufficient training regarding the MHA and 64.7% felt that there should be more extensive training regarding the MHA.
Conclusion
It is crucial to understand the importance of the legislation and the difficulties faced by GPs. Furthermore, it is essential to acknowledge that most GP trainees felt that there should be more extensive education regarding the use of the Mental Health Act 2001.
The current practice of the ICGP involves all trainees participating in a psychiatry rotation to fulfil the criteria of the learning outcomes provided in the curriculum. Additionally, the ICGP has numerous website links which explain how the MHA works and additional documents are provided.
There is also a National Steering Group which compromises representatives from the ICGP, HSE and Mental Health Services. This group focuses on creating distance learning modules through the ICGP and develops resources which can be utilised by GPs and GP trainees alike.
Suggested solutions
There are numerous techniques by which GP trainees can improve their knowledge and confidence regarding the MHA.
Firstly, they could attend the RCPsych workshops or complete online CPD modules.
Secondly, the ICGP could possibly create regular FAQ sessions with GPs and GP trainees. The Mental Health Commission website is another useful source of information.
Finally, to further improve knowledge and confidence regarding the MHA, GPs and GP trainees could apply and study for a postgraduate diploma in Mental Health.
The best way to learn about the Mental Health Act however, is to experience it being used.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)