CARDIOLOGY AND VASCULAR
Acute AF where pulmonary embolism is driving trigger
There is a common association between atrial fibrillation and pulmonary embolism in clinical practice but not in the literature, write Dr Abuelmagd Abdalla and Dr Tom Walsh
November 2, 2016
-
The case of a 94-year-old woman who had an acute pulmonary embolism (PE) manifested as acute atrial fibrillation (AF) with raised d-dimer and troponin but without other clinical symptoms is presented here. She developed transient AF with rapid ventricular response of 160 beats per minute (bpm), however remained haemodynamically stable without requiring defibrillation or thrombolysis.
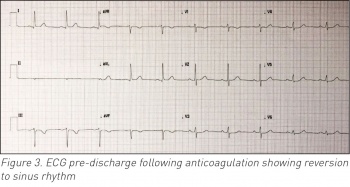
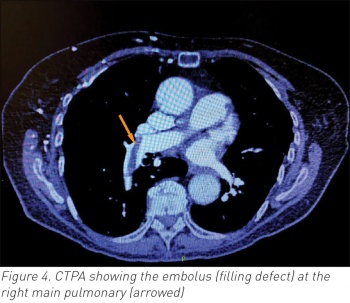
The underlying PE wasn’t diagnosed when she developed AF. She received timely anticoagulation based on already diagnosed subacute deep vein thrombosis (DVT) and her CT pulmonary angiography (CTPA) subsequently confirmed acute embolus in the right main pulmonary artery. Her AF responded well to beta-blocking therapy. The source was right lower limb DVT. Without AF, her PE would have passed unnoticed. The treatment course would have changed acutely if patient had become unstable, but fortunately this wasn’t the case. This case highlights the possible dilemma of treating acute rapid AF that wasn’t primary but rather secondary to an underlying PE.
Background
Pulmonary embolism (PE) is a commonly encountered acute medical emergency. While junior doctors may feel competent to suspect PE in the right clinical setting, it’s becoming more and more complicated and challenging to senior clinicians. There is a spectrum of ECG changes accompanying acute PE, the majority of which are non-specific, especially sinus tachycardia. It’s well known from previous reports that acute right ventricular strain pattern is commonly associated with acute PE.1,2,3 It has also been reported that even ST segment elevation could represent atypical finding in such a setting.4
Troponin leak has also become a known finding accompanying right ventricular stretching. While the causal relationship between atrial fibrillation (AF) and PE has never been established, it’s a common practice for clinicians in acute medicine to suspect PE with new onset AF in those without significant cardiac history. This case highlights the issue of AF as a proxy to underlying potentially fatal PE.
Case presentation
This is a 94-year-old physically well and independent lady who presented with a three week history of right leg swelling that worsened in the past four days, which was confirmed to be due to unprovoked right femoral and popliteal above knee deep vein thrombosis (DVT) by the hospital emergency department. She was admitted medically given her social circumstances and painful leg, and received low molecular weight heparin (LMWH)
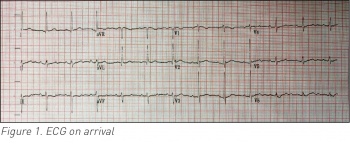
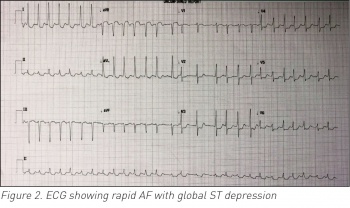
tinzaparin. She was medically stable and her vitals were within normal on arrival. Her chest was clear of focal signs with no signs of cardiac decompensation but her right thigh and calf were swollen and tender.Her electrocardiogram (ECG) on admission was of sinus rhythm and free of acute ischaemic changes (see Figure 1). Of note is that she denied any chest pain or shortness of breath during the preceding period or her hospital stay. Her past medical history was significant for stable angina, hypertension, osteoporosis and peptic ulcer disease. The following day she suddenly developed acute AF with rapid ventricular response of 150-160 beats per minute (bpm) (see Figure 2).
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)