INFECTIOUS DISEASES
RESPIRATORY
Benefits of conscious proning of patients with Covid-19
A team from Portiuncula Hospital discuss the evidence base for the early conscious proning of patients with a Covid-19 diagnosis
August 3, 2020
-
Covid-19 is a novel pathogenic virus caused by Sars-CoV2, severe acute respiratory syndrome coronavirus.1 Most people who are infected with Covid-19 will experience respiratory symptoms but will recover. The HSE estimates about 80% of people will experience the disease as a mild illness and will recover without hospital intervention while a further 14% will experience a more severe illness. Significantly, a further 6% of people will go on to experience a critical illness.2
Sars-CoV2 , may cause acute lung injury and acute respiratory distress syndrome (ARDS). This can lead to respiratory failure and may result in death.
A recent literature review by Diamond et al demonstrated an overall mortality rate for ARDS patients of 43%.3 There is much evidence in the literature in relation to the management of ARDS and there is a rapidly expanding body of evidence in relation to the management of patients diagnosed with Covid-19 who go on to develop ARDS. This article will discuss the experience of conscious proning of a patient diagnosed with Covid-19 on a respiratory ward in a level 3 hospital.
ARDS is characterised by bilateral lung infiltrates and worsening hypoxaemia. It is assessed using a ratio of the patient’s arterial oxygen level (PaO2) to the fraction of oxygen in the air inspired (FiO2). Patients with a PaO2:FiO2 (PFR) of less than 200 are deemed to have severe ARDS.4
Patients diagnosed with Covid-19 who go on to develop severe hypoxaemia notably have little reduction in lung compliance which is in contrast to patients diagnosed with ARDS which is classically characterised by low lung compliance.5 There is a strong evidence base in support of prone positioning of ARDS patients to improve oxygenation.
The PROSEVA ARDS trial confirmed a reduced mortality when proning was introduced and significantly the trial advocates for early implementation of proning. It showed mortality of 16% in proned patients versus 32.8% in supine patients. Data from the UK’s Intensive Care National Audit and Research Centre (ICNARC) observed higher than expected mortality among Covid-19 patients who are mechanically ventilated. This data reports that 66.3% of patients with Covid-19 who required mechanical ventilation died.6
Case study
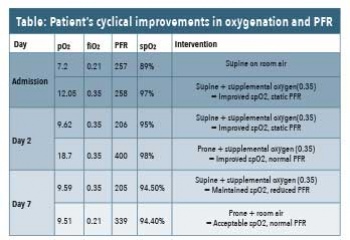
A 59-year-old man presented to the emergency department via his GP with ongoing breathlessness. He had a background history of asthma (British Thoracic Society, level 2 asthma), moderate obstructive sleep apnoea and hypertension. On presentation his chest x-ray showed multilobar bilateral infiltrates. His oxygen saturations were 89% on room air in the ED, with a PFR of 257. A swab confirmed the diagnosis of Covid-19 infection.
On day two of admission he desaturated further requiring > 4Lpm of oxygen to maintain his saturations > 94%. A decision was made to carry out a trial of conscious proning with supplemental oxygen therapy.
In consultation with the respiratory consultant the conscious proning procedure was guided by senior respiratory physiotherapists and the respiratory nurse specialist. The procedure and rationale was fully explained to the patient in order to gain his co-operation. Pillows were placed for self-comfort and proning time was targeted at nine to 10 hours each day (three hours in morning, three hours in afternoon and three hours in evening).
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to aim for prone ventilation for 12-16 hours.7 Despite a shorter proning duration than desired due to staffing constraints at night, the observed physiologic effects of proning on oxygenation were clearly apparent (see Table). Throughout the proning trial the patient was monitored very closely with regular observation of vital signs including oxygen saturations (spO2).
An immediate observation was that proning optimised the ventilation to perfusion ratio (V/Q) which improved oxygenation and PFR (see Table). Despite the fact that initially the patient disliked the periods of time in prone position, he was very motivated by the improvement as he felt much less breathless. This was an important factor in his motivation to continue self proning.
 (click to enlarge)
(click to enlarge)
