CHILD HEALTH
NUTRITION
Common nutritional issues in toddlers: a practical approach
The infant and toddler years present an ideal window of opportunity for obesity prevention, writes Roslyn Tarrant
December 1, 2012
-
Toddler feeding and eating patterns are characterised by increased independence and advancing fine motor control and dexterity that allow them to self-feed. By the end of the first year, toddler developmental and nutritional milestones rapidly progress as they learn to co-ordinate biting, chewing and swallowing, and master self-feeding with hands or spoons, and drink from a cup. From a dental viewpoint in particular, discontinuation of the bottle is recommended from the age of one year.
Typically, the older healthy toddler (over two years) is able to consume most of the foods offered to the rest of the family with some consistency modification to prevent choking/gagging. The specific type of foods offered to toddlers has come into focus with recent Irish data highlighting the importance of the “child’s likes or dislikes” on their level of compliance with a healthy diet.1 Furthermore, “children like what they know, and they eat what they like”2, thus further emphasising the need to foster healthy feeding patterns early on. The toddler will exert their independence and choose what they want; however, it is the job of the parent or caregiver to provide a healthy diet allowing the child to choose from this.
The infancy and toddler years undoubtedly present a potentially ideal window of opportunity for obesity prevention.3 Given that an obese two-year-old is about twice as likely as a non-obese two-year-old to become an obese adult,4 there has never been such a need to convince and educate parents of the importance of complying with toddler healthy eating guidelines. Table 1 outlines some recommendations for practice on nutritional behaviour in healthy young children.
For specific toddler nutritional issues however, tailored nutritional and behavioural modification advice to parents, based on the toddler’s growth/rate, stage of development, feeding ability and presenting condition is required for individual cases.
While an important goal of early childhood nutrition is to develop and establish healthy eating behaviours, the toddler years are often challenging for parents. Applying theory to practice is ‘easier said than done’ for parents who have been provided with advice on feeding their toddler who has suddenly ‘gone off’ their milk, refuses lumpy foods or meat, fruits and vegetables they once consumed without difficulty.
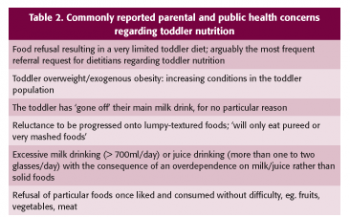
Some of the most commonly reported parental and public health concerns with respect to toddler nutrition are detailed in Table 2. Although any underlying medical condition as a cause of such nutritional issues should be ruled out, generally speaking, many of these feeding issues are largely ‘behavioural’ in nature. It is also noteworthy that these toddler nutritional issues can be inter-related, in that the toddler who consumes excessive volumes of unmodified cow’s milk is more likely to be deficient in iron; those who consume a diet high in sugars (including the excessive ‘juice drinkers’) are at greater risk of dental caries and obesity.
Irrespective of the nutritional issue in question, a careful history and a detailed anthropometric profile (from birth) are integral to the management of toddler nutritional issues. These baseline data are especially important when conditions become persistent and chronic.
Given the adverse effects that, for instance food refusal can have on growth, attention to weight, length/height and head circumference, monitoring is essential to allow for early, and in some cases, more aggressive nutritional intervention. This is of particular importance, since faltering growth may affect up to 5% of the over five-year age group5; it is also known that the earlier growth falters, the poorer the outcome for the child.6
On the other end of the spectrum, with an increasing prevalence of toddler overweight,7 primarily due to an excessive calorie intake in exogenous cases (eg. excessive juice drinking, snacking on high fat/sugar foods), monitoring and early identification of the toddlers ‘at risk’ of overweight and obesity is equally necessary to optimise their outcomes.
Nutritionally assessing the toddler (12-36 months)
The importance of accurately recording and plotting the toddler’s current weight on a calibrated scales (naked weight if less than two years old) as well as their length/height and head circumference, in addition to any previous measurements on an appropriate growth chart cannot be over-emphasised.
When taking toddler length measurements, ideally two individuals are required (and an average of two to three length measurements) both for accuracy and to decrease inter/intra-subject variability; while one individual holds the child’s head against the headboard, the other is required to straighten the child’s knees while holding the feet flat against the footboard.
Anthropometric measurements should be plotted on an appropriate growth centile chart, such as the UK-World Health Organisation growth charts (from zero to four years), which are becoming more widely used in healthcare settings in Ireland, and internationally. For measurement plotting in the toddler up to two years of age the corrected age is used, while uncorrected age/actual chronological age can be used for the over-two-year-old age group.
When tracking toddlers’ weight from their birth weight centile, bear in mind that birth weight is not always a good guide to genetic potential as some infants cross centile lines during the first few months of life. Using the maximum weight achieved between four and eight weeks postpartum is indicated as a more accurate marker of a toddler’s baseline weight percentile.8
In circumstances where there is a concern over poor growth/short stature, it is advisable to compute and plot the mid-parental height and compare the child’s height centile to that of their target height centile range.
Feeding history from birth
In addition to recording the child’s medical, family and social history, profiling their feeding history from birth provides useful baseline information when attempting to understand and address toddler nutritional issues. Detail their early feeding method (breastfed/formula-fed/mixed-fed), if/when breastfeeding discontinued, the types/brands of formula milk consumed from birth (typical volumes consumed/feed frequency) if relevant, the timing of when solid foods were introduced and a note of the type of foods offered.
Delayed introduction to lumpy textured solids (≥ 10 months) for instance, is associated with increased feeding difficulties and more definite food preferences later on.9 Whether any feeding-related conditions were experienced during the first year (include: timing of onset/severity/duration) may also be relevant, including colic, constipation, vomiting (possetting/projectile), reflux or food allergy episodes.
In the older infant/toddler, feeding and social transitions are often associated with the onset of nutritional concerns and fussy eating behaviour, including: weaning off breastfeeding, introducing first solid foods, and transiting from purees to semi-solids to lumpier textures.
When examining the degree to which the nutritional issue is behavioural, it may be relevant to ask who feeds the child, whether they attend a crèche/childcare facility and ascertain if they feed better for one parent/carer than another. Based on parental reports, toddler eating patterns can often improve upon attending a crèche facility where the child is surrounded by other child role models and has to comply with a defined daily meal and snack routine. Information on meal and snack duration is also valuable, as parents frequently report dedicating hours each day to mealtimes, and willing the toddler to eat.
To ascertain the nutrient sufficiency of the toddler’s current diet, and to identify the specific areas to target in advice, it may be worthwhile asking some of the key questions outlined in Table 3.
Food refusal
In our experience, the most frequent dietetic referrals regarding toddler nutrition are associated with food refusal, a concern that often requires long-term intensive dietetic and psychology input for both the parent and child. If the child is thriving however, the first requirement in these situations is to reassure the parent that their child is not undernourished and illustrate this with their comparable weight and length/height centiles.
As long as the child continues to grow normally, no further action is needed.10 In any toddler food refusal case, force feeding is not at all recommended. The parent of the toddler who refuses important food sources such as meat or milk should be reassured that these are usually passing phases and are developmentally normal. In these cases, toddlers quickly learn that mealtimes are ideal attention-seeking time-points which cause major parental anxiety and stress.
If possible, efforts to avoid pandering to the toddler and to minimise attention over food refusal should be encouraged. Dedicating 30 minutes to each main mealtime and around 15 minutes to snack times is an effective first-step measure to implement in the toddler who displays fussy eating behaviour and refuses to eat.
After repeated timely episodes of taking away their meals once uneaten, the toddler will quickly learn to associate mealtimes with eating, rather than attention-seeking events. To optimise the success of this strategy, reiterate to parents that a pattern of ‘grazing’ between meals as the toddler attempts to over-compensate for calories lost during mealtimes, is not recommended. Also impress upon parents that it is very unlikely the child will starve, and if anything, they will be sufficiently hungry for their next meal.
In food refusal cases where the toddler is underweight, advise on offering calorie-dense foods at each meal and snack time, including egg-based meals with added unsalted butter/cheese, full-fat yoghurts, fromage frais with added fruit puree, and added cream to rice or custard puddings. Calorific finger foods including buttered toast/croissant, sausages, cheese cubes, peanut-buttered crackers, pieces of hard-boiled egg, will all help to optimise calorie intake.
To promote weight gain, adding fats such as unsalted butter, oil, mayonnaise, salad cream, cream to foods where possible, should be encouraged (ie. the opposite to healthy eating advice for toddlers, in these particular cases). In the young toddler (up to 18 months), and depending on the severity of the food refusal case, a high calorie formula milk may be necessary.
Nutritionally complete age-appropriate nutritional supplement drinks are also available on prescription (suitable for 8-29kg/in children from one to six years); from a dental perspective, in view of the high sugar content of such supplement drinks, emphasise to parents the need to attend to daily teeth brushing. If toddlers are consuming a daily multivitamin in addition to multiple nutritional supplement drinks, be aware of the potential vitamin/mineral over-supplementation risks. The aim of any additional high-calorie formula/nutritional supplement in the toddler is not to replace main meals, which can easily occur, but to optimise calorie intake, eg. by adding the milk to foods/in meal preparation and as a pre-bedtime drink.
Water can be offered as a supplementary fluid; however, avoid falling into the trap of offering excessive juice and milk volumes (> 500ml/day), as these too can contribute to increased satiety before mealtimes. While tempting to provide sugary drinks and well-tolerated and accepted sugar-laden foods to the toddler, such food choices should not form a major part of the diet since they increase their reluctance to eat other foods, provide ‘empty’ calories, increase satiety and are likely to lead to dental caries.
Part of the management of food refusal in the toddler lies in reassuring and supporting the parent to be consistent and to persist with these strategies; it is equally important that all those who care for the child, including grandparents and extended family, demonstrate a similar approach.
Since it can take up to 12 times of offering a new food to a young child before they will try it, persistence, patience and repeated exposures are likely to lead to eventual acceptance. If a pattern of food refusal persists in spite of the above implemented measures, co-ordinated dietetic, psychology and speech and language input may be indicted. Providing a daily multivitamin and an iron supplement to cover the essential nutrients could also be considered, with any supplements given orally rather than added to the toddler’s food/milk drink.
Excessive milk and juice-drinking
Parents of toddlers who consume excessive milk, juices, and in those whom refuse healthier snack options and ‘will only eat’ snacks such as biscuits and crisps, need to be made aware that such practices are associated with adverse outcomes such as obesity, dental caries, iron deficiency anaemia and constipation.
It will come as no surprise that young children show heightened preferences for sweet, rather than savoury foods.11 Limiting milk volumes to 500ml/day from a cup and offering water as the main toddler supplementary fluid are not only key obesity prevention strategies but also help to increase hunger for meals.
From one year, full-fat cow’s milk can be offered; however, if there is a concern over excess weight gain, low-fat milk can be given in toddlers over two years (skimmed milk only in those over five years). A toddler (1+) formula may be useful in cases where the toddler’s diet is extremely limited and in severe cases of food refusal; however, the goal is always to increase a dependence on solid foods as much as possible, and limit milk drinking to around one pint per day (approx. 500ml max.).
We often find that as soon as the milk volumes are limited, and in particular when any night-time milk feeds are discontinued, toddlers’ intakes of solid foods concurrently increase. If parents wish to offer fruit juice to their toddler, the American Academy of Pediatrics4,12 recommends limiting fruit juice volumes to 120-180ml per day in children from one to six years.
Educating both parents (and grandparents/extended family) on the importance of projecting a consistent and firm message to the toddler, and rewarding positive behaviour when complied with, are all key strategies to implementing any dietary change.
Iron-deficiency anaemia
Iron-deficiency anaemia (IDA) is one of the most common nutritional deficiencies in young children globally. A particularly high prevalence is observed in faltering growth cases (33%),13 as well as those from lower socio-economic groups.
Dietary risk factors for IDA in toddlers/young children include lack of haem iron in the diet from six months postpartum, a dependence on unmodified cow’s milk/juice/tea prior to 12 months, compliance with a restricted diet, faddy eating, and those who experience feeding difficulties. Toddlers who are not progressed onto family foods and meals, and who consume low haem-containing diets (eg. dependence on baby rice, fruit, vegetables) in the absence of supplemented iron are at risk of IDA, as are regular consumers of unfortified cereals/commercial foods. The recommended daily intake for iron in the one-to-three-year-olds in Ireland14 (8mg/day) is comparatively high in relation to the recommended intakes for adult males (10mg/day) and females (14mg/day), placing a high requirement on the early diet to achieve such intakes.
For this reason, a quality toddler diet should include regular sources of haem iron including: red meat, chicken, liver, fish and meat products (eg. black pudding). Also including non-haem dietary sources helps to optimise and maintain iron stores (eg. fortified and wholegrain cereals, pulses, dried fruit, eggs, green vegetables). Avoidance of excessive volumes of milk, especially unmodified cow’s milk, and supplementary fluids such as juices, is recommended for toddlers with IDA in particular.
Depending on the severity of the anaemia, an iron supplement may need to be considered in conjunction with dietary modification. As iron supplements can have side-effects (eg. constipation/nausea/discolouration of teeth), biochemistry monitoring (eg. haemoglobin, ferritin, mean cell volume,) until normal values are achieved is advisable, at which time the iron supplements can be discontinued, with continued biochemistry monitoring as appropriate.
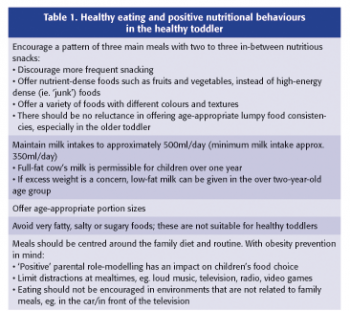 (click to enlarge)
(click to enlarge)

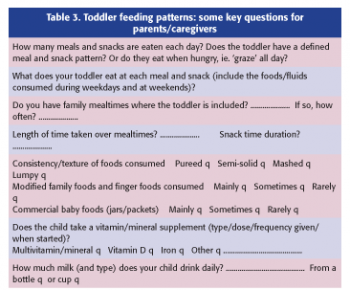 (click to enlarge)
(click to enlarge)