HEALTH SERVICES
Compulsory PCS: What do GPs really think?
A survey has found that most GPs are engaging well with the new PCS, but there remains some confusion around the regime for awarding credits
March 1, 2013
-
Compulsory professional competence is considered relevant in terms of sustained improvement in practice, patient safety, and raising standards of care provided by all practising physicians.1,2 Since May 2011 it has been mandatory for GPs to enroll in the ICGP Professional Competence Scheme (PCS). This study has been undertaken in order to ascertain the initial experience of GPs as users of the scheme, given the importance of the learner feed- back in any educational process. The study also looks to establish the impact of the scheme on GPs, and to provide feedback in guiding future development of the scheme, and meeting educational needs of participants.
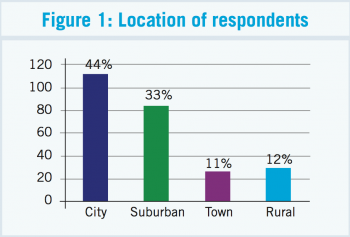
Sampling included GPs from four ICGP faculties (two rural/two urban). The study was conducted with agreement of faculty secretaries. ICGP members were identified from their listing on the ICGP website. Sample size was 362 doctors, equivalent to 14.3% of ICGP membership of 2,515.3 A questionnaire was developed and piloted to establish the uptake, experiences and acceptability of the ICGP CPD Scheme to GPs. It was sent in two mailings (December 2011 and March 2012) to coincide with the end of the first year of the scheme.
A response rate of 71% (257/362) was achieved; 76% (196/257) of respondents worked in urban areas, 74% (190/257) were in a practice with two or more doctors, 93% (238/257) are enrolled in the new scheme and 87% (222/257) were doing an audit.
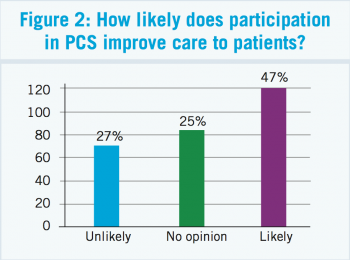
Fifty-six per cent (145/257) of respondents found the PCS fee of €267 unacceptably high. A minority, 34% (133/257) found the system of credits awarded by the scheme clear, 47% (121/257) indicated they believed it would improve the care they deliver, while 38% felt it had increased workload significantly. The results will provide insight into GPs’ experience of the Professional Competence Scheme, and will be relevant to ICGP scheme administrators, as well as reflecting the experience of GPs.
Methods
A postal questionnaire was devised with a view to establishing basic demographic profile, to ascertain uptake of the ICGP administered Professional Competence Scheme and GPs’ opinions of the scheme. Mailing lists were obtained from the ICGP website (December 2011). Four areas were selected; Kerry, Cavan/Monaghan, Dublin South, and Dublin North. The study was discussed and agreed with the relevant faculty secretaries. The questionnaire was piloted (n = 20) for ease of use and clarity, and minimally modified. Pilot data was not included in results.
Mailings were sent out in December 2011 and March 2012. A stamped addressed envelope was enclosed, together with a cover letter explaining the study. Given the survey solicited confidential feedback from GPs only, with no direct patient involvement, no ethical issues were identified.
Results
Profile of respondents and practices
The response rate was 71%, (257 of 362 GPs surveyed), with 76% of responders working in urban areas. Most GPs worked with at least one other doctor (74%). The average reported ratio of medical card patients to private was 56:44. A majority of responding GPs were male (67%), and were aged over 50 years (62%).
In South and North Dublin the response rate was 66.8% (115/172) and 70.5% (79/112) respectively. In Kerry the rate was 80.9% (34/42) and in Cavan/Monaghan it was 80% (29/36).
 (click to enlarge)
(click to enlarge)GPs’ experience with the Professional Competence Scheme
Ninety-three per cent of GPs responding indicated they had enrolled in the scheme, and 87% indicated they were doing an audit. Asked to rate the clarity of the scheme’s system of awarding credits, only 37% indicated it was ‘clear,’ 34% indicated it was ‘unclear,’ with the remainder ‘undecided.’ Just over half (54%) indicated it was likely that GPs would uniformly comply with the scheme. Asked if participation in the scheme would improve the care they provide to their patients, 47% indicated that it would, and 27% indicated it was unlikely to. Most (89%) of responders had logged onto the ICGP website for the purposes of the PCS, but only 46% indicated that it was ‘easy’ to use.
Asked how the scheme has impacted on workload, 48% indicated it had increased workload ‘somewhat’ and 37% felt it had increased workload ‘significantly.’ When asked about the fee of €267, a majority (56%) indicated it to be ‘unacceptably high.’