DIABETES
NUTRITION
Current dietary guidelines in diabetes
It is essential that healthcare professionals are consistent in their dietary advice to patients, and this advice needs to be backed up by evidence
May 27, 2016
-
Media messages pertaining to diet and diabetes feature regularly. With headlines such as ‘Prevent diabetes by eating chocolate’ to ‘Eat to beat diabetes in just eight weeks’ increasingly common, and dietary approaches such as paleo, 5:2 and low carb gaining popularity, is it any wonder that people with diabetes become confused as to what they should or shouldn’t eat to better self-manage their condition?
As healthcare professionals it is essential we keep abreast of the latest evidence, and are consistent in our nutrition messages to support patients in our care in making healthy dietary choices and remaining confident in their self-management.
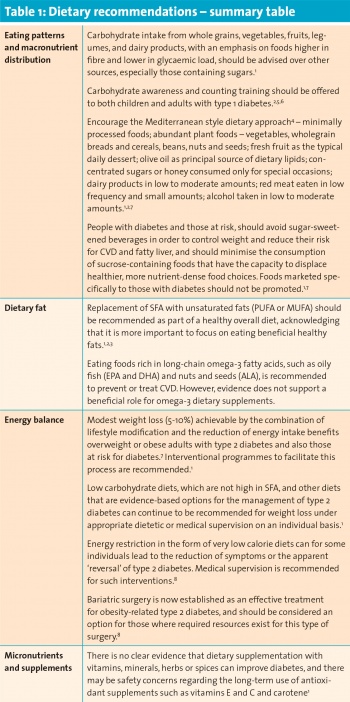
The 2016 American Diabetes Association Standards of medical care in diabetes1 provide us with comprehensive recommendations, each graded into appropriate levels of available evidence. These guidelines state that medical nutrition therapy is an integral component of diabetes prevention, management and self-management education; and that all individuals with diabetes should receive individually tailored advice, preferably provided by a registered dietitian who is knowledgeable and skilled in providing diabetes-specific nutrition advice.
Medical nutrition therapy delivered by a registered dietitian shows A1c decreases of 0.3-1% for people with type 1 diabetes and 0.5-2% for people with type 2 diabetes.1
Importance of structured education
All people with diabetes (type 1 and type 2) should be encouraged to participate in structured education to facilitate the knowledge, skills and ability necessary for diabetes self-care and ongoing self-management. The structured education should be evidence-based, have a structured theory-driven curriculum, be delivered by appropriately trained educators, be quality-assured with outcome measures audited regularly. The education provided should be patient-centred, respectful and responsive to individual patient preferences. It should be outlined to patients at the outset that attendance at and participation in structured education is an integral part of their care.1,6,7
Nutrition and dietary information will form part of this education, with an emphasis in addition on importance of physical activity, footcare, retinal screening and presence or progression of diabetes-related complications.1,8
The overall objective of dietary advice is to assist the person with diabetes to achieve and maintain bodyweight goals, attain individualised glycaemic, blood pressure, and lipid goals and delay or prevent complications of diabetes.1
Individual nutrition needs
During consultations and as opportunity for brief interventions arise, we must also be cognisant of individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthy foods, and motivation and capacity for behaviour change.
As with a population health approach, individuals with diabetes should be encouraged to replace refined carbohydrates and added sugars with whole grains, legumes, vegetables and fruits. We should encourage people to include less saturated fat, replacing with mono- and polyunsaturated fat sources.
The consumption of sugar-sweetened beverages and ‘low-fat’ or ‘fat-free’ products with high amounts of refined grains and added sugars should be discouraged and suggestions provided for suitable alternatives. Sodium intake should be reduced, and tobacco use and excessive use of alcohol should be discouraged.1,4,8
Macronutrient distribution
On average, it has been observed that people with diabetes eat about 45% of their calories from carbohydrate; 36-40% of calories from fat, and the remainder (16-18%) from protein. Although numerous studies have attempted to identify the optimal mix of macronutrients for the meal plans of people with diabetes, a systematic review found that there is no ideal mix that applies broadly and that macronutrient proportions should be individualised.1
Carbohydrate quantities, sources and distribution across the day should be considered, and for those treated with insulin or oral hypoglycaemic agents, timing and dosage of treatment should match quantity of carbohydrate consumed.4 A cornerstone of dietary advice for cardiovascular health has been to reduce the intake of total fat to less than 35% of total energy intake, and to reduce saturated fat (SFA) intake to under 11% of total energy intake.2,4 However, recent research evidence, as well as media coverage, on the type and amount of dietary fat in obesity and the development and management of type 2 diabetes and cardiovascular disease (CVD) has left some healthcare professionals and the general population uncertain about the optimal dietary intake of fat.
Recent debates about the role of high-saturated fat diets in the management of type 2 diabetes have led to concerns about the efficacy of current guidelines as well as the potential risks of high-saturated fat diets. More research is needed before suggesting any major changes to the current healthy eating guidance. Thus, in the absence of evidence for either the superiority or the long-term effects of adopting diets high in saturated fats, they should not be recommended for people with type 2 diabetes.
People with type 1 diabetes are also at an increased risk of cardiovascular disease. Therefore, the general principles of the cardio-protective diet would be sensible as a general recommendation.2 On an ongoing basis we must critically appraise new approaches to diet and determine whether they are likely to benefit or potentially cause harm to certain individuals with diabetes, remembering that evidence-based practice is paramount.
We must clarify and reinforce the basics with patients and refer onwards for dietetic input, structured education or additional support services as appropriate. And ultimately, we must strive to support the needs of each individual patient, acknowledging that there isn’t a uniform dietary approach in the nutritional management of diabetes.
 (click to enlarge)
(click to enlarge)
