DIABETES
OPHTHALMOLOGY
Diabetic retinopathy screening
Conducting a screening programme requires having the capacity and resources in place
August 1, 2013
-
The leading cause of avoidable blindness in adults is diabetic retinopathy (DR) and it is estimated that one person with diabetes per week in Ireland goes blind. With the increasing incidence of new cases of type 2 diabetes currently estimated to be 191,000 patients in Ireland, the prevention of complications is a major issue for the health service. In one UK study of 50,000 type 2 patients, 38% had diabetic retinopathy.1 In another study of 1,688 patients screened, 15% had mild, nonproliferative-to-proliferative retinopathy, nearly 12% required referral to an ophthalmologist, and 5% required urgent referral for potentially sight-threatening retinopathy.2
A study was undertaken to determine what road blocks to diabetic retinopathy screening currently exist in three Limerick GP practices and whether practical steps might be available to prevent new cases of blindness.
Methods
The study was designed to evaluate the efficiency of an Irish diabetic registry utilised in three GP surgeries to track and complete repeated DR screening in every adult patient with diabetes over a recent 18-month period.3 All three surgeries were large, well-established practices with long-term continuity of care by the same GP provider. Each patient record identified on the current diabetes registries was reviewed in autumn 2012. Data extracted into an Excel file included: age, gender, type 1 or 2, date of last DR screen report, and whether DR was found. The DR screen was considered to be complete if an electronic report letter from an eyecare provider was listed in the computerised electronic health record (EHR) documents or a letter dated within the previous 18 months was present in the patient’s paper chart folder.
Results
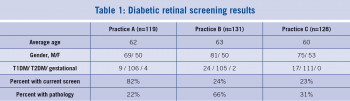
The demographic characteristics of patients between practices were not clinically significantly different. However, a wide gap in the rate of completed and recorded DR screening exams existed between practice A compared to practices B and C. Multiple interfering factors made it unrealistic to expect a rate above 80% for completed screenings. These factors included that not every person with diabetes in receipt of general medical services in the surgery also received diabetes care from the GP. The consultant endocrinologist was responsible for screening patients who were beyond the screening level, some were already in an ophthalmologic consultant’s care for diabetic retinopathy, glaucoma and cataracts. Some referred patients were waiting in the queue or did not keep their last GP booked screening for various reasons. Practices completing less than 50% of screens are eligible for review with the goal of improvement by applying some of the best practices utilised by the best GP practice.
Practice A
In reviewing the diabetic registry of practice A, the retina screening completion rate was above the expected at 82%. The consultant ophthalmologist’s secretary participated in monitoring the recalls and the record of completed screenings. It would be critical for practice A to continue to keep and transmit a timely, current and accurate registry list to the consultant. The 22 unscreened patients with diabetes were evenly divided between men and women, eight were type 1, four had gestational diabetes, and as younger women, probably did not warrant retinal screening at this stage. For the 22 missed recalls, the important issues for improvement was to determine the reasons, such as procedural issues, transportation or other reasons (26%), or to track down patients who were unable to keep scheduled appointments (68% of missed booked screenings) and to remove whatever barriers existed.
Situations that complicated the process included how to screen nursing home patients, prioritising those with multiple major complications which place retina screens further down the list in urgency, and some financial and psychiatric problems that complicate access to screening. Of those 96 patients who had a report letter returned, 22% had developed retinal pathology.
Practice B
The diabetic retinopathy screening rate in practice B was only 24% (32 of 131 charts). The retinal pathology discovery rate was a high 66%, dramatically illustrating the need for a better diabetic retinopathy screening system. Practice B depended on the regional hospital’s ophthalmology department to track and recall their patients with diabetes for retinal screening once initially referred. Several patients went for screening appointments once near their initial diagnosis or entry into the registry, had a good report, and subsequently had not been recalled on a regular basis. Installing a tracking system at the ophthalmological consultant’s level in order to track and recall patients once referred would improve this system.
Practice C
In practice C, patients averaged a little younger, but had about the same mix of more men than women with diabetes, who were mostly type 2. The rate of completed screenings was a disappointingly low 23% (29 of 128 charts). Some 31% had already developed retinal pathology. If the same rate of diabetic retinopathy exists in the unscreened population, at least 30 more patients might have undetected retinopathy in this practice, and the rate of pathology would be expected to increase as the population with diabetes in the practice aged.
Discussion
An improved tracking and recall system that will be practical for all busy GP practices is needed. The difference between practice A compared to practices B and C illustrates the fact that better screening performance is possible. The best models of screening have a designated person in the practice at GP or consultant level who takes primary responsibility for monitoring that the standards of care for the diabetes registry are met as part of their job description. Installing a electronic health record program that would generate reminders is a good step. However, simply installing the program is not enough.4 The computerised system also requires designated staff, training, and monitoring its continuing application. Once operational, the system could also track other diabetic care standards, such as meeting HbA1c goals, the development of microalbuminuria, and routine foot care.
Observations of best practices made during data collection suggest the following future changes in the GP surgery:
- An accurate, updated registry list is basic – a system is required for the surgery’s registration secretary to enter newly diagnosed patients on the registry and delete patients who move or die so that the list remains operational. An alternative would be to cross-check the HSE and insurance billing computers’ summary of all patients given a diagnosis of diabetes at a billed visit/prescription for diabetic medication billed with those who had not had a diabetic retinopathy screening billed within 18 months
- Adding a diabetic quality assurance monitoring sub-routine to the practice computer system works best if a designated, trained person monitors it. Staff members with a friend or family member with diabetes often demonstrate excellent motivation
- Adequate reasons for postponing screening can be recorded as exceptions in the registry; eg. some patients are in long-term hospital or psychiatric care, and some are undergoing surgical shunt procedures or beginning dialysis.
- Potential patient-side or external barriers more likely account for the 12% gap in practice A between arranged screening and completed screenings. Some explanations for these deficits include:
- Lack of motivation for or understanding of the importance of screening
- Solving transportation issues, such as wheelchair needs
- Ability to rebook appointment times if unforeseen circumstances arise
- Ability to meet co-pays or insurance filing requirements.
On the medical system side, since financial constraints currently limit proceeding with the planned full screening programme, a scaled-back procedure may still be helpful. A French study suggests targeting those patients with the longest duration of diabetes and the presence of micro or macro albuminuria who are significantly associated with a higher incidence of retinopathy (p<0.05).5 A Welsh study supports the extension of the diabetic retinopathy screening interval for type 2 diabetes beyond the currently recommended 12-18 months to three years, with the possible exception for those with a diabetes duration of 10 years or more or on insulin treatment.6 Conducting a screening programme also requires having the capacity and resources in place to treat all newly diagnosed diabetic retinopathy in a timely fashion.
References
- Sivaprasad S et al. Ethnic Variations in the Prevalence of Diabetic Retinopathy in People with Diabetes Attending Screening in the United Kingdom. (DRIVE UK), PLoS One, Mar 8, 2012; 7(3):1-6
- Velez R, Tyler M, Chen J, Babcock M, Moran WP. Project I See in NC: Initial results of a program to increase access to retinal examinations among diabetic individuals in North Carolina. N C Med J. Sep-Oct 2011; 72(5):360-4. (Similar statistics found in an extensive study of DR screening in Cork by Buckley C. Evaluation of a community-based diabetic retinopathy screening program, during 2010-2011)
- The study proposal was reviewed and approved by the ICGP ethics committee. Confidentiality of the specific practices and individual data is protected
- Crosson, Jesse C et al. Typical Electronic Health Record Use in Primary Care Practices and the Quality of Diabetes Care. Annals of Family Medicine. May/June 2012: 10(3):221-7
- Perol J, Balkau B, Guillausseau PJ, Massin P. A study of the 3-year incidence of diabetic retinopathy in a French diabetic population seen at Lariboisière Hospital, Paris. Diabetes Metab. Feb 29, 2012; 38(3):225-9
- Thomas RL et al. Incidence of diabetic retinopathy in people with type 2 diabetes mellitus attending the Diabetic Retinopathy Screening Service for Wales: retrospective analysis. BMJ 2012 (Feb 22); (344):874
 (click to enlarge)
(click to enlarge)
