DIABETES
Diet and cultural issues in managing diabetes
A presentation on dietary considerations when managing diabetes patients from different religious and cultural backgrounds
July 1, 2015
-
With over half a million non-Irish nationals living in Ireland,1 it is inevitable that some cultural issues will arise when dealing with medical conditions. Fiona Dunlevy, dietitian manager at St James’s Hospital in Dublin, with several years experience working in the Coombe Hospital, spoke about the dietetic perspective on cultural issues that may arise in diabetes management, at the recent multidisciplinary diabetes study day. She highlighted that the Equal Status Act of 2004,2 has nine grounds of discrimination, namely on: age; disability; gender; sexual orientation; civil status; family status; race; religion; and Traveller grounds.
In her presentation, Ms Dunlevy focused on race and religion, and the set of cultural beliefs and dietary habits that often go hand-in-hand with these, as grounds for issues in diabetes management.
“Religion comes with its own culture. People will have different sets of beliefs or ideals that can actually influence decision-making around their care. Country and nationality are separate to race in many ways, and what people perceive as nationality can be different to what you see on their passport, but it certainly can bring its own set of cultural circumstances,” Ms Dunlevy explained.
The changing demographics of Ireland, and in particular the large Asian and African population that now lives here, will certainly affect diabetes management, also from a dietetic perspective, and how healthcare professionals need to prepare for managing patients.
“A lot of our non-Irish nationals will have diabetes, particularly in pregnancy,” said Ms Dunlevy, who has experience working with pregnant mothers from various backgrounds in the Coombe Hospital.
Tradition
According to Ms Dunlevy, while tradition is a belief or behaviour passed down within a group or society with symbolic meaning or special significance, it is quite often influenced by religion and culture.
“So for example, in parts of Nigeria, it’s considered very rude to look someone in the eye, so this might be misconceived when you have a patient from Nigeria who won’t look you in the eye, or looks away. You might think they’re not listening, but in actual fact they’re just being polite,” explained Ms Dunlevy.
“In other parts of the world, in Japan, crossing your legs and showing the bottom of your foot is considered very rude, something that is very common practice here in Ireland.
“A handshake, which is something we’d all consider part of our culture as a welcome, can in some situations be misconceived. For example, if I as a woman would shake the hand of a muslim man in front of his wife, that could be completely inappropriate to him.
“So we just need to be aware of these things and know that what we might consider being stand-offish behaviour could just be normal behaviour in someone else’s culture.”
Including the family in care
“It’s very important to include families in decisions being made,” said Ms Dunlevy
She explained that this is because while it’s important to put the patient first, over and above the family, a lot of the time the decisions may impact on the rest of the family as well. And if the family isn’t aware of the treatment, particularly when it comes to diet, they might not know what they need to get in the shops or what kind of food to prepare.
“We know the Irish mother has a big influence on what the family will eat. But in Islamic society, the man will often do the shopping. So if we don’t engage him in what needs to be purchased, the wife may lack the right ingredients when cooking for the specific diabetes dietary needs.”
Occasions to be aware of in Ireland
Ms Dunlevy pointed out particular religious occasions, which may influence diabetes management in Ireland. While all cultures and religions may go through times of celebration or festivities, where more amounts or different kinds of foods are enjoyed, the biggest impact on diabetes management is probably Ramadan. This is because it takes place over such a long period of time (a month), and hugely affects food intake.
“Ramadan takes place at different times each year, so this year it takes place from mid-June to mid-July. It involves fasting from sunrise to sunset. In general, it means no food or fluids, and more significantly in relation to diabetes, no medication, including insulin, between sunrise to sunset,” said Ms Dunlevy.
“So if someone is following a fast during Ramadan, it may have a huge impact on their diabetes management.”
Availability of foods
For muslim patients, their diabetes management can be hampered if there is no Halal food available. So for example, if a muslim diabetes patient is hospitalised for a weekend, the lack of Halal food can greatly impact the diabetes management despite the patient still eating.
“Suddenly, the patient may be eating a very carbohydrate-rich diet [sticking to breads, pasta, rice] and hardly any protein [avoiding non-Halal meats], and while this may seem like they are incompliant with the guidelines, the healthcare professional needs to be aware that the patient is just following their religious beliefs, not deliberately trying to be incompliant.”
Hinduism and fast days
In the Hindu religion, there are numerous fast days, Ms Dunlevy explained. These range from fast days where the person with diabetes may just be avoiding meats, to fast days similar to the Ramadan where no food or drink will be taken throughout the day.
“If you have a Hindu patient, I would just advise talking to them about fast days, ask if they are following any fast days and when they plan to do it.”
She stressed again how it is important to be aware of possible food-related management issues and to ask patients about their food habits if there is any chance their food intake can affect the diabetes management.
Case study
Ms Dunlevy presented a case study (see table) and pointed out what needs to be considered in diabetes management when someone intends to fast during Ramadan. In this case, a female with gestational diabetes intended to fast during Ramadan, and brought this up during a consultation.
“Because she was a housewife, I discussed sleeping and taking it easy during the day and almost reversing the day rhythm. The patient followed this plan and was successful, but in particular with gestational diabetes, patients often end up requiring insulin and have to go off the fast anyway,” Ms Dunlevy explained.
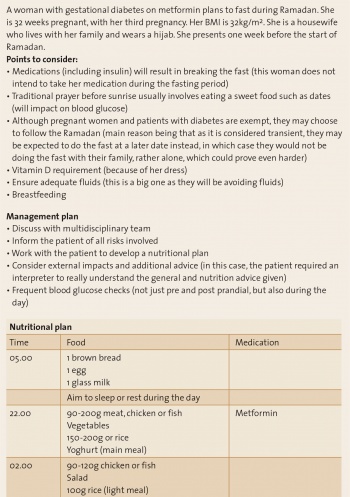 Table. Female with gestational diabetes(click to enlarge)
Table. Female with gestational diabetes(click to enlarge)
