GERIATRIC MEDICINE
RHEUMATOLOGY
Falls prevention: risk assessment and intervention
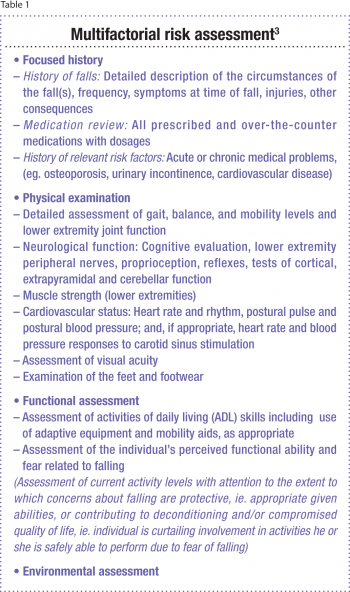
A multifactorial falls risk assessment is recommended for all patients presenting with recurrent falls or difficulties with gait or balance
June 1, 2012
-
Falls are not an inevitable part of the ageing process. However, as we age our risk of falling does increase and, as has been well documented, our population is ageing. Thus a consistently increasing number of our patients are at risk of falls. Currently a third of those over 65 years of age and a half over 80 years fall every year, and of those who do fall, a third will fall again within six months.
With more than 300,000 Irish people aged 50 years and over having osteoporosis, the possibility of many of these falls resulting in fragility fractures is grave. In a person with normal bone mineral density (BMD) a simple fall, that is a fall from a standing height or less, would not result in a fracture.1 But with a diagnosis of osteoporosis (a BMD of 2.5 standard deviations below the mean) the propensity for fragility fractures is acute.
The statistics of recovery from fractures do not make for pleasant reading. Of those who sustain hip fractures for example, less than half will return to their baseline or go directly home, and more than a fifth will require long-term care. Indeed recovery from fractures can often initiate a vicious cycle where an inability to regain baseline function or activity level can lead to an increase in bone loss and in turn an increased risk of fracture.
Falls that do not result in fractures also have serious consequences, including reduced quality of life, fear of falling, reduced confidence and social isolation. Falls are not only associated with morbidity and mortality in the older population, but are also linked to poorer overall functioning and early admission to long-term care facilities.
The current and predicted economic burden of falls in Ireland and internationally is difficult to overlook. The economic burden of illness study conducted by the Irish Centre for Social Gerontology reported that if current trends continue the annual cost of falls and fractures could be €1 billion by 2020 and €2bn by 2030.2
Multifactorial falls risk assessment and intervention
The strategy to prevent falls and fractures in Ireland’s ageing population published in 2008 delineates the lack of integrated service provision in the areas of falls risk screening, assessment and intervention on a comprehensive population basis.
Best practice guidelines outlined in the strategy stipulate that a patient presenting with recurrent falls, an unexplained fall, difficulties with gait or balance, or a fear of falling should have a multifactorial assessment and relevant intervention.
A patient presenting with a single explained fall should have a balance assessment and then either be screened annually for their risk of falling or have a multifactorial assessment and intervention.
The American Geriatrics Society (AGS) and British Geriatrics Society (BGS) updated their clinical practice guidelines for the prevention of falls in older persons in 2010.3 They use a clinical algorithm to describe the process of decision-making and intervention that should occur in the management of older people who present with recurrent falls, with difficulty walking or who present to an emergency department following a fall. The updated guidelines make recommendations in the assessment and intervention process.
In the area of assessment it is recommended that, as well as those who present with a fall and have observed gait and balance problems, patients who simply report difficulties with their gait or balance should have a multifactorial falls risk assessment.3
A falls history should include:
- Frequency of falls
- Symptoms at time of falls
- Any injuries sustained.
In addition, a falls assessment should incorporate:
- Examination of feet and footwear
- A functional assessment, including an individual’s perceived functional ability and fear of falling
- An environmental assessment including home safety.
Intervention
A detailed assessment is of limited clinical use if it does not lead to tailored intervention. The updated BGS/AGS guidelines stress the importance of risk factors identified during assessment being addressed in interventions.
Exercise: Exercise that includes balance, gait and strength training should be included in interventions with community-dwelling older adults.
Environment: Environmental adaptation should follow domiciliary appraisal and should address the safe performance of daily activities as well as fall risk factors.
Vitamin D: Daily vitamin D supplementation is recommended for all older adults at risk of falls, and there is strong evidence to support vitamin D supplementation for older adults with known deficiencies residing in long-term care. In their 2011 report Ross et al concluded that calcium and vitamin D have a key role in skeletal health. The recommended daily allowance (RDA) for men and women over 70 years is 1,200mg/day of calcium and 800IU/day of vitamin D.4
Medication review: Previously medication review was recommended for anyone on four or more medications; now medication review is encouraged for all older people.
Vision and postural hypertension: The importance of vision assessment as part of the overall assessment is highlighted, as is the need to include assessment and treatment of postural hypotension.
Home safety: Home safety assessments are recognised as being a valuable part of a multifactorial falls prevention programme. Persons at risk of falls should have their home environment made safer not only through the removal, replacement or modification of hazards, but also by being taught awareness of hazards and how to avoid them.5 It is also important that assistive devices that are prescribed are used appropriately; otherwise they in turn can become a falls risk.
Community settings
International and national guidelines recommend that those working in the community should ask older people about any falls and undertake a brief mobility screen annually. The need for screening in the community is negated if a patient presents with two or more falls in the previous year, and these patients should proceed directly to having a detailed assessment.3,6
 (click to enlarge)
(click to enlarge)
