PAIN
Fibromyalgia: a challenging diagnosis
While it is now an increasingly more recognised condition, diagnosis and management of fibromyalgia remains challenging for both patient and doctor
March 9, 2018
-
Fibromyalgia has become an increasingly more recognised condition encountered, in particular over the past two decades.1 It is diagnosed in patients who subjectively complain of chronic widespread pain of a ‘burning’ quality of greater than three months. This pain is bilateral, above and below the waist, with multiple tender points, along with a range of symptoms including persistent fatigue, cognitive dysfunction, functional bowel disorder, non-restorative sleep and mood disorder.2,3
It is estimated that 10-20% of the population report some kind of chronic musculoskeletal pain that cannot be traced to a causative factor.4 Statistics for Ireland are limited, but worldwide prevalence of fibromyalgia of 0.4‑9.3% has been reported.5
The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have produced updated guidelines in 2010 and 2016, respectively, for the diagnosis of fibromyalgia.
The ACR 2010 criteria provide a sensitivity and specificity of almost 85% in separating chronic musculoskeletal pain from fibromyalgia. Patients are assessed by using the widespread pain index that divides the body into 19 regions and scores the number of regions that are reported as painful. The symptom severity score then assesses severity of fatigue, unrefreshing sleep and cognitive symptoms. Both the widespread pain index (maximum 19) and symptom severity scores (maximum 12) are combined into a single questionnaire with scores from 0 to a maximum of 31. A modified and more useful version of the ACR 2010 allows for direct patient administration.6
Who gets fibromyalgia?
Historically, women were assumed to be more commonly affected by fibromyalgia.7 A study from Minnesota, US found that 4.9% of men and 7.7% of women fulfilled the criteria for a diagnosis of fibromyalgia, however only 27% of these were given a diagnosis of the condition. The analysis further concluded that only 2% of women and 0.15% of men were actually medically diagnosed with fibromyalgia.7
What causes fibromyalgia?
The exact cause of fibromyalgia is not yet known. Although no structural or functional abnormalities in the muscle tissue are appreciated, increasing evidence does support dysfunctional pain processing in the nervous system, with amplification of pain signals as a key mechanism in the development of fibromyalgia.7
Abnormal signalling in the pain and emotion processing centres of the brain such as the thalamus, amygdala and insula have been demonstrated on functional magnetic imaging studies.7 A likely genetic predisposition has also been identified in familial studies where one quarter of relatives of fibromyalgia patients reported chronic widespread musculoskeletal pain.1
Although no one specific gene has been shown to be responsible, emerging evidence is strong for a polygenic effect with genes affecting the catecholamine, dopamine and serotonin pathways playing a role and predisposing patients to a dysfunctional stress response, as well as triggering the clinical symptoms of fibromyalgia.1 Psychosocial distress has also been shown to influence the development of chronic pain associated with fibromyalgia. The biopsychosocial model could therefore explain the expression of fibromyalgia from its likely genetic factors, to triggers and other factors such as mood disorder, maladaptive behaviour and socio-economic status, which can collectively influence the chronicity of symptoms.
Why and how should fibromyalgia be diagnosed?
The diagnosis and management of fibromyalgia is challenging for both the patient and clinician. It often takes more than two years for a diagnosis to be made, with the patient having been seen on average 3.7 times for consultations with different physicians.8 This can put a huge financial burden on the healthcare system. Data suggest that in the US total annual costs for patients with fibromyalgia average approximately $6,000, compared to an average of $2,000 for those in the general patient population.5 It is important to note that as well as the direct expenditure on medical care and treatment, non-medical costs, including those incurred by the patient and lost productivity from work, should also be taken into consideration.
The care of patients with fibromyalgia ideally starts in the primary care setting, where the professionals will have a good knowledge of patients from the biopsychosocial perspective as well as providing primary care over a prolonged period of time. Therefore, the primary care setting should be the focal point of management. An early and positive diagnosis could reduce costs by avoiding unnecessary testing, imaging, medication use, specialist referrals and primary care visits.
The diagnosis of fibromyalgia is based mostly on a clinical evaluation and simple blood tests. Although testing for the typical 18 sites for tenderness as specified by the ACR is helpful, it should not be used to confirm the diagnosis as the examination alone is mainly a subjective exercise. It is reported that 25% of patients diagnosed with fibromyalgia do not have 11 tender points.7 However, asking the patient about associated symptoms, including non-restorative sleep, poor concentration and fatigue, in the setting of chronic widespread pain strongly suggests a diagnosis of fibromyalgia.
Only simple blood tests like FBC, U&E, TFTs (to rule out hypothyroidism), ESR, CRP, a comprehensive metabolic panel and fasting glucose test are needed.
Vitamin D levels could also be taken because vitamin D deficiency can aggravate pain, although it does not cause it.9 Antibodies such as ANA, RF and anti-CCP may be requested if the examination suggests an autoimmune cause. Specialist consultation should be sought if symptoms suggest an alternative diagnosis.
Management and treatment of fibromyalgia
There is no cure for fibromyalgia and treatment should aim towards reducing symptoms, with the goal of the patient reaching optimal function in daily life. Management of symptoms should take into consideration the fluctuating and heterogenous nature of symptoms in a multimodal, patient-tailored approach.1 Patient education is important; diagnosis and an explanation for the symptoms should reassure patients that they do not have a more severe illness.1 This would hopefully reduce the need for unnecessary investigations.7
Recent EULAR guidelines recommend focusing on pain, fatigue, sleep and daily functioning. These recommendations are evidence-based, can be tailored to the individual patient ,and include both pharmacological and non-pharmacological therapies.
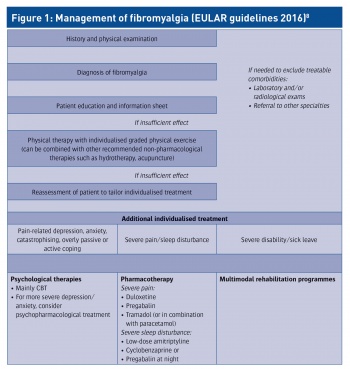
The EULAR guidelines, shown in Figure 1, suggest a graduated approach, beginning with non-pharmacological therapies such as exercise, with an individualised pharmacological plan thereafter for the treatment of either severe pain or sleep disturbance (or both if they are present). Psychological therapies are included in updated guidelines and include education and cognitive behavioural therapy (CBT).8,9
Non-pharmacological
- Active therapy including aerobic exercise (20 minutes/day, two to three times a week)
- Passive therapy including balneotherapy (heated spa or pool treatment), massage, manipulation
Psychological
- Education to explain symptoms and mechanisms of fibromyalgia
- CBT to help reduce pain with focus on what links pain, thought (mood) and behaviour (negative coping strategies).
Pharmacological
- Antidepressant – amitriptyline 10-50mg
- Anticonvulsant – pregabalin 300-600mg
- Serotonin-norepinephrine reuptake inhibitor – duloxetine 60-120mg
- Tramadol and paracetamol combination – tramadol 37.5mg or paracetamol 325mg four times per day.
Experience at a clinical level involves starting amitriptyline 7.5mg nocte, titrating up to 50mg (if needed) per night optimal for pain and sleep relief. Pregabalin can be started at 25mg, twice daily for pain and anxiety, titrating up as needed. Side-effects can be an initial complaint with pregabalin, especially with increased sensitivity to alcohol.
Sleep hygiene is imperative, as patients with disturbed sleep patterns and lifestyle changes often experience increased fatigue, which might result in non-compliance. Care should be taken with prescribing medications such as opiates and neuroleptics due to their addictive nature.
 (click to enlarge)
(click to enlarge)
