DIABETES
Good technique means good control
Using the correct injection technique is key in ensuring optimal glycaemic control in patients
March 1, 2017
-
Diabetes is a worldwide public health challenge, with the number of adults diagnosed with diabetes now reaching 415 million worldwide.1 In Ireland, an estimated 225,840 people are living with diabetes and that number is set to rise.2 However, if treated and managed correctly, people with diabetes can lead very active and healthy lives.
It is well established that improving glycaemic control reduces the risk of people with diabetes developing long-term complications; the Diabetes Control and Complications Trial (DCCT) showed that keeping blood glucose levels as close to normal as possible slows the onset and progression of the eye, kidney, and nerve damage caused by type 1 diabetes3 while the UK Prospective Diabetes Study (UKPDS) showed conclusively that the complications of type 2 diabetes could be reduced by improving blood glucose control.4 In the longer-term, poor glycaemic control can increase the risk of complications including kidney failure, blindness and limb amputation, all of which have a devastating impact for the individual.5
Healthcare workers can help people with diabetes to achieve optimum glycaemic control (and thus avoid complications) through encouraging the active management of their condition. This includes having an effective exercise regime and a managed diet, making sure that glycaemic levels are optimally managed, but also, for patients using insulin injection therapy, having a good injection technique that leads to accurate insulin delivery.
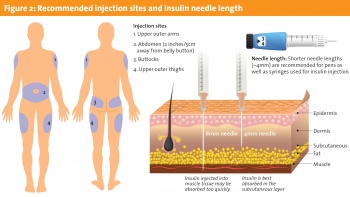
Correct injection technique (IT) is crucial for injectable therapies like insulin to achieve optimal glycaemic control. A number of factors contribute to good IT including the injection process, needle length, and the rotation of injection sites.6
Informed healthcare workers can educate people with diabetes on correct injection technique, improving personal patient outcomes and encouraging on-going management of their condition. The following case study of one patient shows the significant positive impact the injection technique and active condition management can have.
Case study
This case study concerns a 32-year-old woman who has been living with type 1 diabetes for 16 years. Her last severe episode of hypoglycaemia was in 2007; she presented for preconceptual care in December 2014 following a miscarriage earlier that year.
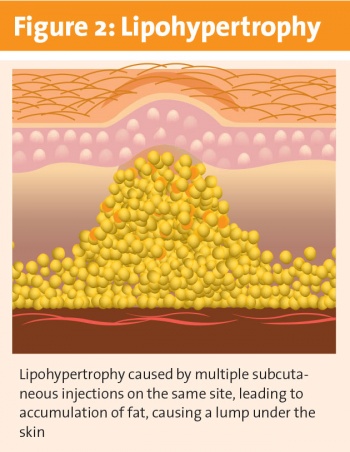
Despite living with diabetes for 16 years, discussion revealed that her knowledge of self-care and condition management was outdated. She was using an 8mm needle and failing to rotate injection sites. She also routinely injected into areas of lipohypertrophy (a rubbery tissue growth under the skin7) and 50% of her glucose levels were above targets.
The patient was advised to follow best practice injection technique, including rotating injection sites, using a 5mm needle and avoiding injections into lipohypertrophy. In the six months following this advice, only 10% of her daily control glucose levels were above targets and her insulin usage dropped by 18 units from an original total daily dose of 76 units.
Following this intervention, the patient was in a better position to improve her glycaemic control for pregnancy; she achieved a pregnancy in 2015 and delivered a healthy baby girl in December 2015.
Best practice injection technique
As this case study shows, a number of factors contribute to good injection technique and improved glycaemic control, including needle length and the rotation of injection sites.6 Informed healthcare workers can educate people with diabetes on correct injection technique, improving personal patient outcomes.
For reliable absorption, insulin should be injected into the subcutaneous fat layer. This allows it to be absorbed at a more predictable rate, which can lead to more stable glycaemic control.8 If insulin is injected intramuscularly it may be absorbed too quickly, leading to greater glycaemic variability and potentially an increased risk of hypoglycaemia.9 However, it makes no difference whether insulin is injected into deep or shallow subcutaneous tissue; it is absorbed at a similar rate.10
While subcutaneous depth can vary from person to person, skin thickness ranges from 1.2-3mm regardless of gender, age, BMI or ethnicity.11 Short (4mm or 5mm) pen needles are appropriate for use for everyone carrying out insulin injection as they simplify injection technique (no need for a skin-fold in most cases) and will consistently pass through the skin to the subcutaneous layer and reliably deposit insulin with low risk of intramuscular injection (see Figure 1).12

 (click to enlarge)
(click to enlarge)