INFECTIOUS DISEASES
HIV and hepatitis C co-infection
The emergence of hepatitis C co-infection as a major ongoing cause of morbidity and mortality, even in those with well controlled HIV infection
March 3, 2014
-
Even in those with well controlled HIV infection, hepatitis C co-infection as a major ongoing cause of morbidity and mortality related to liver disease has become an area of renewed focus and interest in recent years. This is due to the development of new directly acting agents against hepatitis C virus (HCV) and the promise of greater cure rates in a HIV-infected patient group and with greater insights into optimal ways to manage HIV/hepatitis C co-infection. This article aims to review the current concepts related to HIV/hepatitis C co-infection in terms of acute HCV infection in HIV-positive patients, transmission of hepatitis C and treatment strategies in those with HIV and hepatitis C co‑infection.
Hepatitis C
Hepatitis C exists in six genotypes (1-6) and over 50 genotypic subtypes. In Ireland the majority of infections are related to genotype 1 although genotype 3 is increasingly common. There are no major differences in the clinical course among the various genotypes but the response to interferon-based therapy differs significantly, with genotypes 2 and 3 being more responsive than 1 and 4.
Like HIV, HCV is also a ribonucleic acid (RNA) virus although they belong to differing viral families (Retroviridae and Flaviviridae, respectively). HCV replicates rapidly causing many viral mutants and through this mechanism can evade the body’s immune response and establish chronic infection. Unlike HIV, however, viral replication is in the hepatocyte cytoplasm and therefore the viral genome is not incorporated into the hepatocyte, which means there is the potential for its clearance from the plasma completely and hence spontaneous clearance of infection.
Acute HCV infection in the general population is symptomatic in 25-35% of people. However, in the HIV-infected population this is much less and if symptomatic it is often very mild or goes unnoticed due to altered immune responses. This phase of acute HCV infection is defined as the first six months after infection, during which time the liver transaminases tend to rise rapidly before declining again and may reach normal levels. In non-HIV-infected patients estimates of clearance following acute HCV infection are 15-45% whereas in HIV-infected patients this is as low as 10%. Factors such as CD4 counts at the time of HCV infection impact on this further, reflecting again the altered immune response to HCV infection.
There is much debate about the treatment of acute HCV infection in HIV-infected patients and studies have shown success rates of up to 70% for those treated in the acute phase. Therefore, most guidelines support treatment of acute HCV infection in HIV co-infected patients.
Transmission of infection
The predominant mode of HCV transmission is parenteral, with up to 80% of injecting drug users infected. Transmission risk relates not only to the sharing of needles but also other equipment, including tourniquets, cooking gear, water, syringes etc. The rates of HCV co-infection among HIV-infected patients with injecting drug users (IDU) as the mode of acquisition is as high as 95%. Sexual transmission of HCV is harder to define in terms of exact risk.
Some studies have shown in the MSM community (men who have sex with men) with HIV infection, 75% of HCV seroconversion occurred by non-parenteral routes, with particular sexual practices being associated with increased transmission risk (traumatic anal intercourse, ‘fisting’ and ‘rimming’ practices). The overall rate of HIV/HCV co-infection in this population is approximately 10%. Perinatal transmission of HCV infection is significantly increased in infants born to a HIV-infected mother, with a fivefold increase in risk in this group (4-7% versus 20%). Overall, approximately one-third of HIV patients are co-infected with HCV.
Chronic HCV infection causes inflammation and lymphocytic infiltration in the liver, particularly of the portal tracts as well as both focal and bridging necrosis and fibrosis. In mono-infected patients 10-15% will progress to cirrhosis after 20 years of untreated infection. Hepatocellular carcinoma (HCC) occurs at a rate of 0-3% per year in the setting of cirrhosis. HIV infection impacts on the rate of progression to both cirrhosis and the risk of development of HCC and liver-related death. For this reason an early diagnosis of HCV co-infection and prompt staging and treatment where appropriate is vital in HIV-infected patients.
All HIV-infected patients should be screened for HCV co-infection and those with high risk ongoing behaviours should have annual HCV-antibody testing performed. Those found to have chronic HCV on testing should have quantification of HCV RNA and assessment of genotype as these will impact on treatment decisions. In those with a high likelihood of achieving treatment success for HCV (defined as those with a sustained virological [SVR] response six months after therapy completion) include genotype 2 or 3 and a low HCV RNA at baseline. Liver biopsy is not always necessary, especially in the presence of normal liver ultrasonography.
Therapy decisions
In genotype 1 HCV infection, recent studies have shown the usefulness of the blood test IL28B in guiding probability of treatment success. Genetic variants near interleukin 28B which encode interferon-gamma 3 were associated with a favourable response to interferon therapy, specifically the CC genotype as opposed to the CT/TT genotypes. This has proven to be especially important in HIV/HCV co-infected patients with a twofold higher rate of SVR in the IL28B CC group.
Considerations prior to deciding to commence HCV therapy in HIV co-infected patients are similar as for mono-infected patients in terms of contraindications to therapy. Patients at greatest risk for progression to end-stage liver disease should be considered for therapy.
Factors related to progression to cirrhosis
- Male sex
- Alcohol use > 30g/day men, 20g/day women
- Older age at infection (> 40 years)
- Portal or bridging fibrosis or at least moderate necrosis on biopsy (> grade 2)
- Tri-infection with HBV/HIV/HCV
- Persistent elevation of ALT/AST.
Factors related to treatment success
- Genotype 2 or 3
- Low-level HCV RNA at baseline (HCV RNA < 800,000)
- Age < 40
- Duration of disease more than five years
- Absence of significant fibrosis on biopsy
- Absence of hepatosteatosis
- Abstinence from alcohol
- Insulin responsiveness.
In those for whom HCV treatment is deferred, repeat liver biopsy should be considered every three to five years as in HIV/HCV co-infected patients as histological damage occurs at rates greater than in those who are mono-infected and may also progress despite the absence of abnormal liver transaminases. Over the past two to three years there has been a growing trend in evidence which suggests that highly active antiretroviral therapy (HAART) may improve outcomes in HIV/HCV co-infected patients.
However, it is not as yet an indication to start HAART. The decision regarding timing of therapy for HCV in the co-infected patient should be taken into consideration early even in those whose HCV therapy is to be deferred, as initial choice of antiretrovirals will be impacted upon by the current or future need for HCV therapy due to certain cumulative drug toxicities.
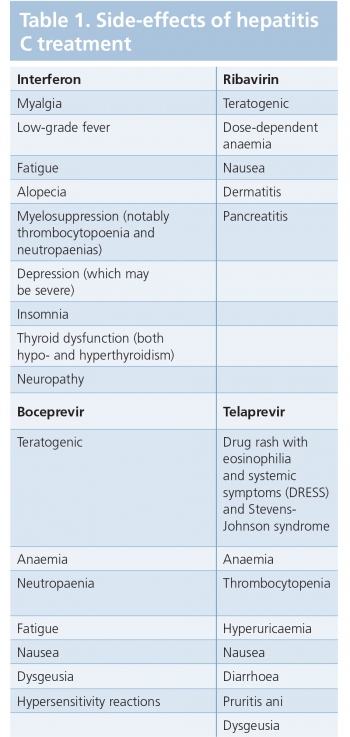
For example, zidovudine, an antiretroviral agent, causes anaemia and leukopaenia and the addition of ribavirin and interferon will further potentiate this effect. Toxicity is also important when it comes to women of child-bearing age and two forms of contraception must be used due to the teratogenicity of ribavirin.
In the case of women on HAART this often will mean two forms of non-hormonal contraception as most oral contraceptives and depot preparations undergo drug-drug interactions with antiretroviral medications and may not be as effective.
Treatment regimes for HCV in HIV-infected patients
The primary goal in HCV therapy for chronic hepatitis C is eradication of HCV from the serum, as determined by undetectable HCV RNA. The secondary goal is reduction in the amount of hepatic inflammation/fibrosis with the expectation of decreased disease progression and subsequent reduction in HCC risk.
Pegylated-interferon is the interferon of choice as it has covalently bound molecules of polythene glycol allowing weekly dosing by subcutaneous injection. This is given in combination with ribavirin. For HIV-infected patients with HCV genotype 2 or 3; the standard duration of treatment is 48 weeks. This differs from HIV-negative patients as studies have shown higher relapse rates with the standard 24 weeks therapy offered to HCV mono-infected patients.
The duration of therapy also depends on the response to treatment. Patients with a < 2 log decline from their baseline HCV RNA should have their therapy discontinued as they are considered a treatment failure. Those with HCV RNA detectable at 24 weeks should also have treatment discontinued and be considered treatment failures.
HCV genotype 1
HCV infection with genotype 1 is managed differently than 2 and 3 due to the development of new directly acting antiviral agents (DAAs). These are inhibitors of HCV proteases or polymerases. The two currently licensed DAAs are boceprevir and telaprevir, which act against an HCV-encoded serine protease required for cleavage of the viral polyprotein during and after translation. This causes potent inhibition of viral replication. Unfortunately, single point mutations in the viral genome lead to the emergence of high level resistance to these agents that precludes their use as monotherapy. They are both currently licensed to be given in combination with pegylated interferon and ribavirin as standard of care.
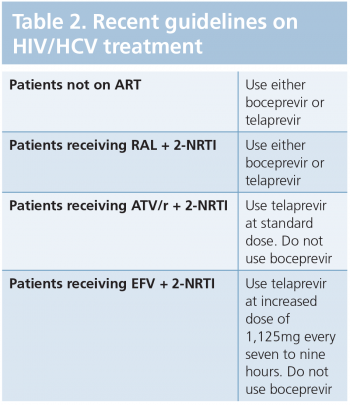
The choice of DAA in HIV/HCV co-infected patients will largely depend on the HAART regimen the patient is receiving. If a patient is not on HAART or is on HAART consisting of a dual NRTI backbone in combination with the integrase inhibitor raltegravir, either DAA may be safely used. Those on a dual NRTI backbone in combination with boosted atazanavir or efavirenz must use telaprevir (upward dose adjustment for telaprevir with efavirenz owing to drug-drug interactions). No other HAART regimens are advised at present owing mainly to the large number of drug-drug interactions between the two classes.
Data on which to base definitive recommendations on dosing and duration of therapy in co-infected patients is lacking, therefore the current recommendations are as that for monotherapy, although guidance tends towards a 48-week therapy course in co-infection, regardless of the week 4 and 12 viral load results, while further studies are being done.
Boceprevir-based therapy
A four-week lead-in with standard of care therapy with weight-based ribavirin and pegylated interferon is commenced followed by boceprevir being added at week four. If HCV RNA at week four of triple therapy is undetectable, then 20 weeks of triple therapy with RIB plus IFN plus boceprevir is the recommended duration. If HCV RNA is detectable at week four, boceprevir is continued to week 36 of triple therapy and standard of care therapy continued for the final 12 weeks to a total of 48 weeks therapy.
All patients with cirrhotic liver disease should have 48 weeks of therapy with boceprevir administered to at least week 36 and ideally to week 48. In those previously treated for HCV who relapsed or were non-responders, they should have four-week lead-in with standard of care therapy and then triple therapy to week 48 regardless of the week eight data. If the HCV RNA measure is > 100 at week 12, therapy should be discontinued
Telaprevir-based therapy
Telaprevir is commenced alongside standard of care therapy with RIB plus IFN for the initial 12 weeks of therapy and following this a response-guided duration of therapy is used. If the HCV RNA is negative at four and 12 weeks, then 24 weeks total therapy of RIB plus IFN can be given. If HCV RNA is detectable at these time points, 48 weeks of therapy should be used. All patients with cirrhotic liver disease should have 48 weeks therapy as well as null or partial responders on prior treatment.
If the HCV RNA is > 1,000 at four or 12 weeks, then therapy should be discontinued. This tablet is formulated into a 375mg tablet and two pills three times daily with a moderately fatty meal is the recommended dosage.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)