RHEUMATOLOGY
NUTRITION
Importance of adequate oral vitamin D intake for bone health
While the main source of vitamin D is sunlight, oral sources have primacy in both the correction and prevention of vitamin D deficiency
September 1, 2012
-
Vitamin D is the name given to a group of fat soluble steroids, the two major physiologically relevant forms of which are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol).
Sources and metabolism of vitamin D
Unlike other nutrients, vitamin D is a conditionally required nutrient being obtained from two sources – predominantly by skin production upon exposure to natural ultraviolet (UV) solar radiation, and to a lesser extent by oral intake. Being a fat soluble vitamin, it has a long half-life of about two weeks and is stored in fat tissues.
For nearly six months of the year from October to March in Ireland, skin production of vitamin D is absent and the population is dependent on oral intake from natural foodstuffs (which are consumed in small quantities only), fortified foodstuffs (most notably some milk products for the past 25 years) and vitamin D supplements, either in multivitamin tablets or in combination with calcium tablets.
Vitamin D is carried in the bloodstream to the liver, where it is enzymatically converted to 25-hydroxyvitamin D (25OHD). Further hydroxylation by the kidney results in the formation of the active form of the vitamin: 1,25-dihydroxyvitamin D [1,25(OH)2D]. This is the hormonal form of vitamin D; its production is tightly regulated by parathyroid hormone (PTH) and the recently described phosphate-regulating hormone, fibroblast growth factor 23 (FGF23). The hormonal form promotes absorption of both calcium and phosphorus from the small intestine.
The hormonal form is also produced in other tissues in the body, such as the placenta during pregnancy, skin, gastrointestinal tract, lymphatic tissue, prostate and breast. At these sites, it is thought that 1,25(OH)2D only has a local effect. But overproduction such as in diseases like sarcoidosis and lymphoma may cause hypercalcaemia. Also, it is thought that this local production and action of 1,25(OH)2D may have other beneficial effects (see ‘Health consequences’ below).
Assessment of vitamin D status
The serum concentration of 25OHD is typically used to determine vitamin D status. It reflects vitamin D produced in the skin as well as that acquired from the diet, and has a fairly long circulating half-life of 15 days. It does not, however, reveal the amount of vitamin D stored in other body tissues.
The measurement of serum 25OHD is technically complex and as with any analytical technique the value delivered by laboratories is only an estimation of the true value, due to inherent measurement uncertainty. Nonetheless, assays of high standard for 25OHD are now widely available in Ireland. The key challenge is the correct interpretation of the 25OHD result. First, it must be understood that the 25OHD result is a measure of supply but is not an indicator of disease. A result should never be used to state that a patient has ‘vitamin D deficiency’, although this is commonly misstated in clinical practice. Essentially, it is a measure of supply and estimate of risk of bone disease. It is also an excellent means of assessing compliance for those on supplementation.
The simplest interpretation of a serum 25OHD result in line with an international report from the Institute of Medicine (IOM)1 is:
- A level below 30nmol/L indicates risk of disease
- A level of 30-50nmol/L is satisfactory for the population at large
- A level above 50nmol/L guarantees adequacy in 97.5% of the population.
Any individual who is sun deprived is at risk of low vitamin D status. Predisposing factors contributing to risk of deficiency include age, ethnicity linked to wearing concealing clothing, residential latitude and seasonal differences in solar UVB availability. In Europe and Ireland in particular, our high residential latitude puts children and adults at high risk of 25OHD deficiency. Also at risk are pregnant and lactating women and their infants.
Recommended dietary intakes for North Americans
The IOM in North America, covering the US and Canada, recently updated its 1997 dietary reference intakes for both calcium and vitamin D for all life stages, except infants (see Table 1 and 2). It used two terms: the estimated average requirement (EAR), which specifies the average requirement; and the recommended daily allowance (RDA), which specifies the requirement that meets the needs of 97.5% of the population.
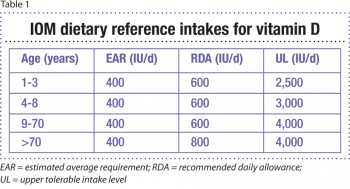 (click to enlarge)
(click to enlarge)

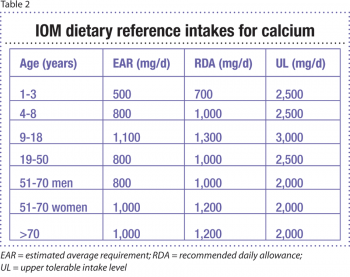 (click to enlarge)
(click to enlarge)