GENERAL MEDICINE
Infusion therapy moves into the community
The delivery of community-based infusion services is gradually gaining pace in Ireland
July 1, 2011
-
Intravenous (IV) therapy as we know it today is a highly specialised form of treatment that provides a quick and effective method of delivering medication, fluids, total parenteral nutrition and blood products.
Although the practice of using veins to inject substances essentially began in the 17th century, the major advances in IV therapy occurred during the past 150 years – evolving from an extreme measure used only on the most critically ill to a therapy used for almost 90% of all hospitalised patients.
However, IV drug infusion therapy is not confined solely to the hospital setting. Demands for acute hospital beds, advances in treatment regimens, changes in government policy and greater patient participation in treatment decisions are challenging the traditional perception that infusion therapy should be confined to the hospital environment.
Increased IV use in community care
IV therapies are now increasingly being delivered in community settings, including skilled nursing facilities, health clinics and patients’ homes. Indeed, the practice settings for IV therapy delivery are as varied as the patient populations served by this speciality; from the hospitalised neonatal patient to the geriatric patient in a nursing home, all patients assessed by their doctors as being unable to have oral medication, or where medication via the intravenous route is deemed to be the treatment of choice.
The Infusion Nurse Society (INS), which is the recognised global authority in infusion therapy, encapsulates the diversity of IV therapy settings and treatments: “In a clinical setting one might find the nurse transfusing blood products and interpreting haemodynamic data gained from IV monitoring. Another nurse may be training a mother to administer total parenteral nutrition to her toddler in a suburban home. A colleague is fighting downtown traffic to reach a working executive in time to change a cassette on an ambulatory antibiotic pump, while yet another is recommending vascular access devices to the new oncology patient in the physician’s office.”
Bernadette Carter, who is one of the founding members of the Irish and UK International Affiliate of the INS, says tens of thousands of patients across a range of diseases such as cancer, rheumatology, respiratory, cystic fibrosis, gastro disorders and many infectious diseases rely on infusion treatment.
“The list of innovative medications is growing, patients have more medical options than ever before and our nurses play a vital role in getting these medicines to them,” she remarks.
Infusion therapy may be provided for patients who need:
- Medication for chronic illnesses such as Crohn’s disease, bronchial asthma and diabetes
- Pain management
- IV hydration therapy
- Blood products such as platelets, red cells or plasma
- Low-dose chemotherapy
- IV antibiotics for an infection
- Post-transplant IV medications
- Immunomodulators (drugs that stimulate the immune system)
- Biological response modifiers (substances made by living cells that stimulate the body’s response to infection and disease; used for rheumatoid arthritis and other conditions)
- IV anti-emetics for nausea and vomiting
- IV immune globulin to boost the body’s natural defence system against infection
- Monoclonal antibodies to suppress the immune system or to kill/inhibit cancer cells
- Therapeutic phlebotomy, which involves withdrawing a prescribed amount of blood to improve the symptoms of a blood disorder.
Infusion teams typically include a doctor who writes a prescription and develops a schedule for infusions, and infusion therapy nurses who actually perform the treatments and monitor the patients while treatment is ongoing. The medication can be delivered directly into the body via a blood vessel, the spinal cord or a muscle.
Ms Carter explains that, up until recent years, the management of this highly specialised treatment area has been under the care of individual hospitals rather than one overarching body.
However, the arrival of the INS in Ireland in 2010 supports nurses and healthcare professionals through establishing standards, educational programmes, publications and access to experts in infusion care.
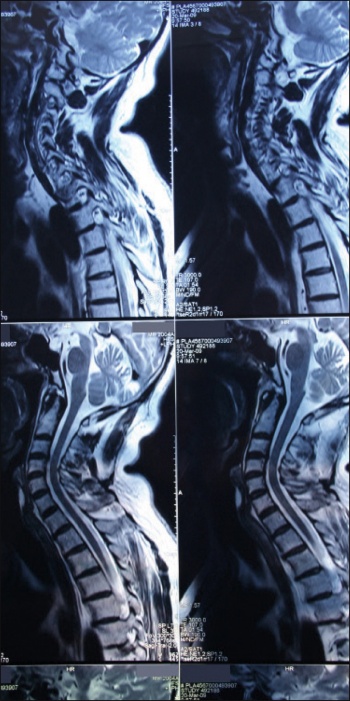 MRI is the most effective way of showing whether a patient’s back pain is amenable to minimally invasive surgery, according to neurosurgeon Mr Steven Young(click to enlarge)
MRI is the most effective way of showing whether a patient’s back pain is amenable to minimally invasive surgery, according to neurosurgeon Mr Steven Young(click to enlarge)
