CANCER
Lung cancer – think inside the cell
Small molecule TKIs have had a significant impact on the treatment of lung cancer
February 3, 2015
-
Each day, patients with lung cancer arrive at specialist cancer centres all across Ireland to receive treatment; some are post-op and adjuvant, others have stage IV disease. All are hopeful.
“The surgeon said it has all gone nurse, the chemo is just for insurance.”
“It has come back nurse, but I’ll fight it again.”
“I need more chemo, I need more radiotherapy.”
These are familiar patient comments to nurses working in oncology. Chemotherapy and radiotherapy schedules are well understood by staff and are explained daily to patients and relatives. Targeted cancer therapies are now also commonly used to treat this disease, but are we as knowledgeable when explaining these drug regimens to patients? Are there gaps in our knowledge?
What of the community pharmacists, who are often the most accessible healthcare professionals, are they meeting patients who have questions about these targeted cancer drugs? Public health nurses provide vital community support for cancer patients. Do these professionals have educational needs also?
This article aims to explore the benefits and challenges of small molecule tyrosine kinase inhibitors (TKIs), and provide a learning opportunity for all professionals caring for patients with lung cancer who have been prescribed a TKI.
Then and now
The last decade has witnessed the development of targeted therapies, such as erlotinib, gefitinib, afatinib and crizotinib, which have revolutionised the way patients with lung cancer are treated. However, when I started my oncology career over 15 years ago, targeted therapies were virtually unheard of. Patients had surgery, chemotherapy and radiotherapy in varying combinations depending on their disease stage.
This is still the case today, but scientific research has devised new drugs that target specific cell activities, which are now valuable additions to the lung cancer treatment armamentarium.
Better toxicity profile than conventional chemotherapy, better target selectivity, availability for chronic treatment and, in some cases, oral administration have marked these targeted compounds as the most promising research drugs.1
Oncology nurses are familiar with the increasingly important role of targeted treatment, such as tyrosine kinase inhibitors, epidermal growth factor receptor- (EGFR) directed mutations or angiogenesis inhibition, particularly in the area of non small-cell lung cancer (NSCLC), which represents approximately 85% of all lung cancer diagnoses.1 Understanding of these novel targeted therapies is growing but is it robust enough for the patient who asks: “Is there a targeted therapy for my type of cancer?”
Keeping abreast of new agents and clinical trials is a challenge. ‘Mabs’ (monoclonal antibodies) and ‘Ibs’ (small molecule inhibitors) seem to be growing in numbers and coming onto the market relatively quickly. While many medical oncology conferences are focusing on new molecular targets, already delegates, such as those addressing the ASCO 2014 lung cancer round-up,2 are discussing how to overcome resistance to targeted therapies. Just as we are learning how these novel treatments work, a new wave of research is developing next generation inhibitors for next generation mutations. Updates and highlights are needed constantly.
Benefits and challenges
A frequent advantage attributed to these targeted therapies for NSCLC is that most of the small-molecule TKIs are administered orally.
The Cancer Information Support Network3 describes how patients will spend less time in oncology units and will be spared intravenous discomfort and associated risks. This is extremely important especially in the context of a group of patients who may have advanced disease with poor prognosis.
Patients can take these sophisticated drugs at home, which can offer improved quality of life and reduce costs for both patient and hospital.
Clinical trials have shown positive results for patients in terms of response rates, progression-free survival and overall survival compared to standard chemotherapy, and these are clear advantages. Molecular targeted therapies are also perceived to be less toxic generally, although some patients are sensitive to these drugs and can develop substantial side-effects.4
“The research team found that erlotinib did help stop the cancer growing in some people, but that it didn’t always help people live longer. They found that erlotinib worked better for those who developed a rash during treatment.”5
“Afatinib demonstrated modest but noteworthy efficacy in patients with NSCLC who had received third- or fourth-line treatment and who progressed while receiving erlotinib and/or gefitinib, including those with acquired resistance to erlotinib, gefitinib, or both.”6
“Gefitinib improves progression-free survival for metastatic lung cancers with EGFR mutations.”7
“Results from an international phase III trial show that crizotinib (Xalkori) may benefit previously treated patients with advanced lung cancer whose tumours have a specific genetic mutation.”8
What are the challenges?
Costs
Unfortunately, costs to the state for these drugs are very high. High-tech drug costs for the top 10 TKIs in 2012 exceeded €20 million. While not all of this expense was related to lung cancer treatment, overall, TKIs are very costly.9
Adherence
“Drugs don’t work in patients who don’t take them.” C Everett Koop MD
Patients have increased responsibility for their treatment, and compliance with medication is crucial. The British National Formulary (BNF) 201010 emphasises the importance of patients understanding the purpose and side-effects of, and even how to take, their medicines, or poor compliance can follow. Agreement between the prescriber and the patient on desired health outcomes should be reached.
The BNF recognises that time is needed to explain potential side-effects to patients and their families, and that pharmacists can re-emphasise the instructions given by the direct healthcare team. However, not all patients are compliant and I have had experience of some not even collecting their prescriptions.
The benefit of knowing our patients’ personalities and abilities should be taken into consideration when prescribing any medication, and it is clearly crucial with regard to targeted therapies as the impact of non-adherence may be very serious for NSCLC. It is also important to establish who the medication manager is for a patient, as often times it is a relative. Accurate, clear instructions about the daily administration of a specific target therapy are required from all professionals meeting the patient or their relative to avoid poor outcomes. Issues such as what time should the medicine be taken at? Should the medicine be taken with or without food? What to do if a dose is missed? All of this advice needs to be explained.
Side-effects
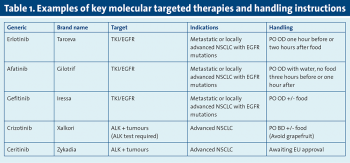
Lung cancer patients have benefited from advances in treatment with the arrival of many small molecule TKIs that work inside the cancer cell on a pathway or mutation, eg. the epidermal growth factor receptor (EGFR). Some key molecular-targeted therapies, their indications and handling instructions, are detailed in Table 1.
Side effects include:
Skin toxicities
- Diarrhoea and other GI disturbances
- Electrolyte changes (K+ MgSO4)
- Hyperglycaemia
- Hyperlipidaemia
- Mucosal changes
- Hypertension
- Arterial thrombotic/thromboembolic events
- Cardiac toxicities
- Wound healing
- Bowel perforation
- Interstitial lung disease
- Proteinuria.
 (click to enlarge)
(click to enlarge)
