MEN'S HEALTH I
Male sexual dysfunction
The GP should be receptive to both the overt and the oblique or disguised reference that may be made about a patient’s sexual difficulties, as opportunity may present for an important intervention
August 1, 2013
-
Many GPs can be reluctant to engage with their male patients on the topic of the patient’s sexuality. There are many reasons for this reluctance, including lack of time, embarrassment (both doctor and patient), lack of knowledge about male sexual dysfunction and the doctor’s reluctance to invade on the patient’s privacy. While these are all understandable sentiments, we may be missing an opportunity to make a real, valid and important intervention that could make a significant difference to the patient’s wellbeing.
GPs should also understand that permission to discuss should be bi-directional – the patient may need permission to understand that discussion relating to sexual issues is allowed in the GP’s surgery and the GP should ascertain that permission to discuss sexual issues with a patient is forthcoming.
The GP should also consider, with the patient’s permission, the early introduction of the partner into the therapeutic relationship. It is surprising how often the male who has a dysfunction is under the delusion that his partner may not have noticed ‘his’ problem. It is almost invariable, where a dysfunction exists, that the partner suffers at least some emotional distress as a result of the dysfunctional sexual relationship. Ignoring the partner’s involvement may complicate therapeutic resolution or recovery at a later date. Additionally, some therapeutic modalities may require the cooperation and/or involvement of the partner. The GP should consider methods to allow the tactful integration of the partner into the therapeutic relationship from an early stage.
It is helpful if the GP understands his or her own biases and comfort levels when discussing potentially controversial issues such as extramarital sex and relationships, sexual abuse, termination of pregnancy, same-sex relationships, bisexuality, transgender issues and unusual sexual ideation and/or practices.
The GP should be receptive to both the overt and the oblique or disguised reference that may be made about a patient’s sexual difficulties. The information may come from the sufferer or his partner. Simple enquiries may quickly reveal an obvious dysfunction or elicit an indirect reference to information that may need to be explored at a later consultation either by the GP or by another practitioner with greater or more focused expertise.
The sexually competent male must:
- Have libido (desire or interest for his sexual partner)
- Be psychologically comfortable with his current sexual activity and his ability to perform that activity
- Be able to divert blood from his iliac artery into his corpora cavernosa and keep it there for a sufficient length of time to achieve penile tumescence/rigidity and hence an erection adequate for penetration
- Be able to discharge semen through his urethra (ejaculation)
- Be able to experience a sense of pleasure (orgasm).
Most (but not all) male sexual dysfunction involves a failure of one or more of the above processes.
The Massachusetts Male Ageing Study (MMAS), published in 1994, suggests that male sexual dysfunction first emerges as a common problem for men in their early 40s and increases with advancing age. At age 40, 40% of men acknowledged some impairment of sexual function and this impairment increased by approximately 10% with each successive decade.1
Loss of or decreased libido
Loss of or decreased libido is sometimes revealed by the sexual partner of the man and may be caused by many different factors:
- Normal ageing
- Relationship problems
- Androgen deficiency
- Depression
- Stress/fatigue/anxiety
- Recreational drugs/alcohol abuse
- Medication (SSRIs, antiandrogens, 5-alpha reductase inhibitors and opiates)
- Systemic illness
- Body image difficulties with self or partner,
- eg. colostomy, mastectomy etc
- Psychological factors, including hypoactive sexual disorder, sexual aversion disorder, distorted body image and other sexual dysfunctions (eg. fear of humiliation)
Psychological comfort
Comfort with his current sexual activity is a prerequisite for a man’s successful performance. A man must be confident with his circumstances, be emotionally/physically/sexually attracted to his current partner and have reasonable confidence in his ability to perform sexual activity. Wide ranges of unhelpful psychological interventions in this thinking are often grouped together under the umbrella term ‘performance anxiety’. Examples include a new partner, previous erection failure and disorders of sexual orientation.
Much has been written about the effect of pornography, widely available on the internet and elsewhere, on the development, orientation and maturation of the male psyche. Many views have been expressed, but no consensus reached, regarding influence of pornography on the aetiology of sexual aggression. Sex addiction, usually but not exclusively a male phenomenon, is now widely recognised for its harmful effects that may rival or occasionally exceed those of alcohol and illicit drugs.
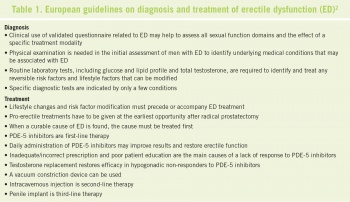
Erectile dysfunction
Erectile dysfunction (ED) is defined as the consistent or recurrent inability to acquire or sustain sufficient rigidity and duration for sexual activity.
The causes of ED may be physical, psychogenic but may often be both. Pointers to a psychogenic cause include younger age, sudden rather than gradual onset and significant use of the internet or other sources of pornography. Hair restoration and transplant clinics often prescribe finasteride, which has been found to induce impotence in up to 18% of users.
A multinational study of 27,839 men in eight countries (US, UK, France, Italy, Spain, Germany, Mexico and Brazil) ranging in age from 20-75 years showed that the overall incidence of ED was 16%. ED ranged from 8% of men in the 20-30 years age group and climbed to 37% of men in the 70-75 years age group.3
Another study demonstrated that obesity, smoking, watching television and the presence of comorbid conditions were associated with a higher risk of ED. Exercise, weight loss and physical leanness are associated with an improvement in ED in about one third of patients.4,5
Numerous studies6-10 have also identified risk factors for ED which include:
- Age
- Diabetes mellitus
- Hypertension
- Obesity
- Dyslipidaemia
- Cigarette smoking
- Sleep apnoea
- Intercourse frequency < 1/week.
It can be seen that cardiovascular disease and ED have many risk factors in common and endothelial dysfunction may be the common link.11,12 GPs should be aware that ED may be an early warning sign of cardiovascular disease and conversely, cardiovascular disease may coexist with ED.
It has been widely believed that many drugs are associated with ED. Many antihypertensive medications, particularly beta blockers, were thought to have a contributory effect to ED but in the Treatment of Mild Hypertension Study trial, only the thiazide diuretic, chlorthalidone, was shown to produce a higher incidence of ED than placebo.13 Other commonly prescribed medications that list ED as a side-effect include antidepressants (especially SSRIs), spironolactone, clonidine, guanethidine, methyldopa, ketoconazole and cimetidine (but not ranitidine or famotidine).
Physical conditions including pelvic trauma, stroke, spinal cord or back injury, multiple sclerosis, dementia and pelvic surgery (including prostate surgery) may all cause ED. Other infrequent causes of ED include cycling, hyperprolactinaemia, hyperthyroidism, hypothyroidism and hypogonadism.
Treatments for ED should be targeted at the perceived cause of the problem. Psychiatric or psychological problems should always be looked for and addressed. Lifestyle modification to include quitting smoking, dietary modification and weight loss and regular exercise should be considered first-line therapy. In general, the PDE-5 inhibitors, sildenafil, tadalafil and vardenafil are safe and often effective treatments for many men who have ED, provided the prescribing guidelines are closely followed.
Occasionally, testosterone replacement therapy is indicated for a hypogonadal patient but the therapeutic effects for ED in these men are greater when testosterone and a PDE–5 inhibitor are co-prescribed.14 Prescribers should exercise caution when using testosterone alone as it may restore or increase desire but do little or nothing for performance.
Other medications that can be used to treat ED include alprostadil, which can be given as an interurethral pellet (MUSE – not currently available in Ireland) or as an injection (Caverject), which is injected into the dorso-lateral aspect of the proximal third of the penis.
Ejaculatory disorders
Ejaculatory disorders is the term given to a heterogeneous collection that includes premature, delayed absent and retrograde ejaculation.
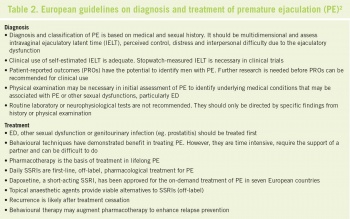
Premature ejaculation
Premature ejaculation (PE) must have three essential criteria for diagnosis:15
- Ejaculation which always or nearly always occurs prior to or within about one minute of vaginal penetration – intra-vaginal ejaculatory latent time (IELT)
- The inability to delay ejaculation on all or nearly all vaginal penetrations
- Negative personal consequences such as distress, bother, frustration, and/or the avoidance of sexual intimacy.
The aetiology of PE is not known or is obscure in most cases. Negative psychological conditioning, learned behaviour, genetics and genital hypersensitivity might be factors, although none of the theories is supported by quality experimental data. PE can be further classified into symptom-based subtypes that include acquired versus lifelong PE, global versus situational PE, and PE coexisting with other sexual dysfunctions, especially ED.
The exact prevalence of PE is difficult to define but it is a common finding in couples with relationship and/or sexual difficulties. Anecdotal evidence suggests that PE is not an unusual factor in infertility investigation of couples. Further anecdotal evidence suggests it may also be associated with sexual problems in the partner, particularly anorgasmia, sexual pain disorder and vaginismus.
About 30% of men with PE have concurrent ED, which typically results in early ejaculation with a limited or absent erection.
Treatments for PE can be divided into four broad categories:
- Psychotherapeutic intervention can, with time and partner cooperation, be effective and may also be useful where there are associated sexual difficulties in both partners
- The so-called ‘squeeze technique’ is a simple and sometimes effective adjunct to therapy in a cooperative sexual relationship
- The local application of a lidocaine-prilocaine anaesthetic solution under a condom has been found to be effective for some men in the treatment of PE16
- Pharmacological treatments for PE are supported by robust evidence. The efficacy of off-label use of SSRIs (paroxetine, sertraline, citalopram, fluoxetine and the serotonergic tricyclic, clomipramine) has been known for some time. Dapoxetine is a novel SSRI with a short half-life that has recently received a licence as an on-demand treatment for both lifelong and acquired PE, to be used 1-3 hours before anticipated sexual activity.
The on-demand approach overcomes many of the difficulties that PE sufferers have with daily dosing of an ‘antidepressant’ and dapoxetine has been shown to significantly improve intra-vaginal ejaculatory latent time, perceived control and satisfaction with sexual intercourse, and to also reduce personal distress and interpersonal difficulties.17
The evidence supporting the efficacy of PDE-5 inhibitors, using either on-demand or daily dosing in the treatment of PE is contradictory. There is evidence for their use where PE and ED are comorbidities.15
Delayed ejaculation, anejaculation, retrograde ejaculation and male anorgasmia
These are included in a spectrum of disorders that are probably beyond the scope of most GPs. It should be noted, however, that the beneficial effects of SSRIs in PE might produce unwanted anorgasmia when treating either men or women, and delayed or anejaculation when treating men for anxiety and/or depression. The patient should always be warned of this possible side-effect.
GP management
The initial approach to a man with any of the common sexual dysfunctions should always include the taking of an appropriate history and a focused physical examination. Examination of the external genitalia is mandatory as certain conditions such as Peyronie’s disease (growth of fibrous plaques in the penile tunica albuginea causing abnormal penile curvature, penile pain and erectile dysfunction) and physical hypogonadism may need targeted treatment, quite separate from the presenting complaint.
Biochemical investigation for straightforward sexual dysfunction in men can usually be limited to a morning serum testosterone, lipid analysis, thyroid function tests, fasting glucose, prolactin and serum creatinine.
Glucose and lipid analysis are likely to have a high yield and, while specific therapy may not be relevant for the sexual dysfunction on their own merits, they may require management to prevent associated long-term morbidity.
Two other useful adjuncts for the GP who may be faced with a more complicated male sexual dysfunction are a urological surgeon with an interest in the area and/or a psychotherapist who is skilled in the art of single person or couple sexual therapy.
References
- Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994; 151(1):54
- Wespes E, Amar E, Eardley I, Giuliano F et al. Guidelines on Male Sexual Dysfunction: Erectile dysfunction and premature ejaculation. European Association of Urology 2012; http://www.uroweb.org/gls/pdf/13_Male%20Sexual%20Dysfunction_LR%20II.pdf
- Rosen RC, Fisher WA, Eardley I, Niederberger C, Nadel A, Sand M. The multinational Men’s Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Men’s Attitudes to Life Events and Sexuality (MALES) Study. Curr Med Res Opin 2004; 20(5):607.
- Bacon CG, Mittleman MA, Kawachi I, Giovannucci E, Glasser DB, Rimm EB. Sexual function in men older than 50 years of age: results from the health professionals follow-up study. Ann Intern Med 2003; 139(3):161
- Esposito K, Giugliano F, Di Palo C, Giugliano G et al. Effect of lifestyle changes on erectile dysfunction in obese men: a randomized controlled trial. JAMA 2004; 291(24):2978
- Fung MM, Bettencourt R, Barrett-Connor E. Heart disease risk factors predict erectile dysfunction 25 years later: the Rancho Bernardo Study. J Am Coll Cardiol 2004; 43(8):1405
- Sullivan ME, Keoghane SR, Miller MA. Vascular risk factors and erectile dysfunction. BJU Int 2001; 87(9):838
- Chiurlia E, D’Amico R, Ratti C, Granata AR, Romagnoli R, Modena MG. Subclinical coronary artery atherosclerosis in patients with erectile dysfunction. J Am Coll Cardiol 2005; 46(8):1503
- Mannino DM, Klevens RM, Flanders WD. Cigarette smoking: an independent risk factor for impotence? Am J Epidemiol 1994; 140(11):1003
- Grover SA, Lowensteyn I, Kaouache M, Marchand S et al. The prevalence of erectile dysfunction in the primary care setting: importance of risk factors for diabetes and vascular disease. Arch Intern Med 2006; 166(2):213
- Sullivan ME, Keoghane SR, Miller MA. Vascular risk factors and erectile dysfunction. BJU Int. 2001; 87(9):838
- Chiurlia E, D’Amico R, Ratti C, Granata AR, Romagnoli R, Modena MG. Subclinical coronary artery atherosclerosis in patients with erectile dysfunction. J Am Coll Cardiol 2005;46(8):1503
- Grimm RH Jr, Grandits GA, Prineas RJ, McDonald RH et al. Long-term effects on sexual function of five antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women. Treatment of Mild Hypertension Study (TOMHS). Hypertension 1997; 29(1 Pt 1):8
- Rochira V, Balestrieri A, Madeo B, Granata AR, Carani C. Sildenafil improves sleep-related erections in hypogonadal men: evidence from a randomized, placebo-controlled, crossover study of a synergic role for both testosterone and sildenafil on penile erections. J Androl 2006; 27(2):165.
- Althof SE, Abdo CH, Dean J, Hackett G et al. International Society for Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation. International Society for Sexual Medicine. J Sex Med 2010; 7(9):2947
- Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: a double-blind, randomized, placebo-controlled study. BJU Int 2004 May; 93(7):1018-21
- McMahon CG, Althof SE, Kaufman JM, Buvat J et al. Efficacy and safety of dapoxetine for the treatment of premature ejaculation: integrated analysis of results from five phase 3 trials. J Sex Med 2011 Feb; 8(2):524-39
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)