MENTAL HEALTH
Managing insomnia – careful and detailed assessment is vital
Sleep related disorders are very common, with insomnia affecting most people at some stage in life
July 13, 2016
-
Insomnia is from the Latin in somnus meaning ‘without sleep’ and is defined as a lack of sleep due to insufficient sleep quality or quantity. The other major criteria for the diagnosis of insomnia as outlined in the DSM-5 are:
• One or more of difficulty initiating sleep, difficulty maintaining sleep or early morning awakening (more than 30 minutes than desired) with the inability to go back to sleep
• The sleep disturbance causes significant distress or impairment in social, occupational, educational, academic, behavioural or other important areas of functioning
• The sleep difficulty occurs at least three nights per week, is present for at least three months, and despite adequate opportunity for sleep
• The insomnia does not co-occur with another sleep-wake disorder
• The insomnia is not explained by coexisting mental disorders, medical conditions or the physiological effects of a substance.
The DSM-4 distinction into primary and secondary criteria is removed in DSM-5 which highlights the comorbid nature of insomnia, emphasising the need for treatment of both insomnia and the medical disorder.1
Insomnia can be classified as transient, acute or chronic. Transient insomnia persists for less than a week and may be caused by another disorder, changes in the sleep environment, depression or stress. Acute insomnia, also known as stress related insomnia, is the failure to sleep well for less than a month while chronic insomnia lasts for longer than a month.2
Sleep-related disorders are remarkably common and insomnia affects most people at some stage in life which is often stress related. Management is often challenging and requires a careful and detailed assessment. The Irish Sleep Society states that sleep-related medical disorders are also highly prevalent, particularly obstructive sleep apnoea, which affects at least 4% of adults.3
Epidemiology
While studies vary, it is reported that insomnia occurs in one-third of the general adult population. Approximately 10-15% of patients with current complaints of insomnia will be classified as suffering a moderate to severe disorder.4
Increased age, marital separation and divorced or widowed status are risk factors. Other studies have shown that limited years of education, low income and unemployment may also increase insomnia risk. There is a higher prevalence in women which increases with age due to the effects of menopause. Symptomatic treatment for complaints such as hot flushes does not always lead to resolution of symptoms. Patients with comorbid medical and psychiatric conditions are at significant increased risk, with psychiatric and chronic pain disorders having insomnia rates as high as 50-75%. Incidentally, insomniacs have a threefold increased risk of suicide attempt.2
Stress is another common precipitating factor with epidemiologic studies showing increased stress levels in the workplace associated with higher rates of sleep complaints. Shift workers are also at higher risk of insomnia reflective of their circadian rhythm disturbances.2
Assessment and investigations
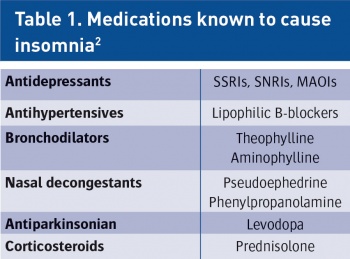
Assessing a patient presenting with insomnia requires a detailed exploration of their medical (eg. dementia, thyroid disease, Parkinson’s disease), psychiatric, psychological and social history in order to out rule other conditions that may be causing the insomnia. Common comorbid psychiatric conditions include mood disorders and anxiety disorders. The Irish Sleep Society guidelines recommend full physical and mental state examinations along with a full sleep history when there is a complaint of chronic insomnia. A comprehensive sleep history should include sleep habits, sleep environment, caffeine intake, medications (prescription and non-prescription), substance abuse, alcohol and smoking history.3 Table 1 outlines the common medications that can cause insomnia.
Patients should be encouraged to keep a sleep diary for two weeks to determine their sleep pattern. The diary should include time to bed, total sleep time, time to sleep onset, number of awakenings, use of sleep medications, time of awakening and subjective feelings in the morning. There are also various sleep questionnaires to assess sleep quality and duration such as the Epworth sleepiness scale which is useful in diagnosing sleep disorders such as OSA and monitoring response to treatment. If a sleep related disorder is suspected it is important to enquire about the relevant symptoms such as snoring or apnoeic episodes (OSA) and leg jerks or kicks (restless leg syndrome/periodic limb movement disorder). Collateral history from a bed partner is often particularly valuable but not always confirmatory.3
Blood tests for hyperthyroidism and low ferritin levels, which can cause restless legs, may be warranted. An FBC may rule out anaemia. Polysomnographic data/sleep studies or multiple sleep latency tests are not routinely preformed in the diagnostic work up of insomnia. However in cases where sleep-disordered breathing, narcolepsy, nocturnal movement disorder or parainsomnia are suspected they are indicated.3
Non-pharmacological management
Interestingly, non-pharmacological measures have comparable efficacy to hypnotic medication for insomnia and may have more long-lasting effects. Hypnotic medication is recommended only for short-term use due to dependency, with rebound withdrawal effects upon cessation and drug tolerance. Non-pharmacological management as detailed below is therefore recommended first-line and provides long lasting improvements to insomnia. Any identifiable underlying causes of insomnia should be treated first where possible such as pain, depression, anxiety disorders and physical symptoms (eg. wheeze, dyspnoea, nocturia).3
Sleep hygiene advice
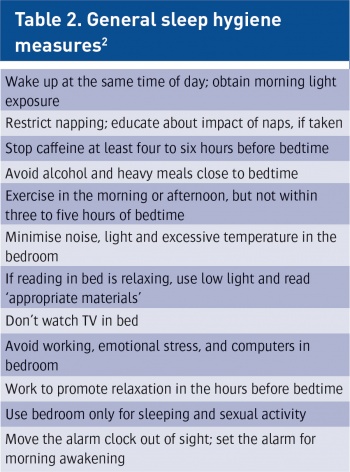
All patients suffering from insomnia should receive education on sleep hygiene. There is insufficient evidence for use as monotherapy, but it is crucial in conjunction with other measures. Patients should be advised on healthy sleeping behaviours and preferable environmental conditions such as light, noise, temperature and bedroom environment. They should also be counselled on lifestyle factors such as exercise, diet and use of caffeine, alcohol and cigarettes.3 Table 2 outlines important general sleep hygiene measures.
Relaxation therapy
These relaxation techniques are designed to reduce somatic tension and intrusive thoughts interfering with sleep. Progressive muscle relaxation and imagery training comprise some of the techniques used, which aim to reduce physiological arousal, eliminate intrusive thoughts and reduce worry. Wind-down routines before bedtime also help to reduce anxiety before sleep.3
Sleep restriction
Sleep restriction therapy is based on an assumption that sleep deprivation will promote a stronger drive to fall and remain asleep.2 It improves insomnia by restricting the time allocated for sleep each night so that the time spent in bed correlates with the individual’s presumed sleep requirement. This therapy may take at least several weeks before significant changes are noted by the patient. Time in bed (TIB) should not be below five hours per night and once the sleep efficiency has reached 90%, TIB can be increased gradually by 15 minutes per week until the optimal sleep has been achieved.3 A sleep efficiency of 80% to 85% is considered optimal. More than 90% may indicate sleep deprivation, and below 75% is considered to be a sign of poor quality sleep.5
Stimulus control therapy
Patients are given a set of instructions designed to reinforce the association between bed and sleep with the aim of re-establishing a consistent sleep wake cycle. These instructions include:
• Only go to bed when sleepy
• No reading, watching TV, listening to radio or using phones or smart devices in bed
• Time to get up should be the same seven days a week regardless of the amount of sleep the night before
• 15 minute rule: the patient should be told to get out of bed if they are awake for 15 minutes and go to another part of the house (not another bedroom). They should only return to bed when sleepy
• Avoid daytime napping.3
Cognitive behavioural therapy
CBT has been found in meta-analysis to be as effective as medication for the short-term treatment of chronic insomnia. The favourable effects may persist well beyond completing therapy, in contrast to those produced by medication.6 However, behavioural therapies are often not adequately tried depending on access to local resources.
CBT attempts to address maladaptive behaviours and thought patterns aiming to teach patients improved sleep habits and relieve their counter-productive assumptions about sleep. Common treatment targets include unrealistic sleep expectations (‘I must get eight hours sleep a night’), misconceptions about insomnia causes, worrying about the consequences of insomnia (‘I cannot do anything after a poor night’s sleep’) and performance anxiety about trying to get a good night’s sleep.2
Pharmacological management
Hypnotics should be the last option rather than the first for management of insomnia. Medication is indicated when the insomnia is severe, disabling or subjecting the patient to extreme distress.
Benzodiazepines
Benzodiazepines have been used as sedative hypnotics for decades and have been demonstrated to be safe and effective in the treatment of insomnia, but are restricted to short-term use.2 When commencing sedative hypnotics, treatment should be for a limited duration (two to four weeks) at the lowest effective dose. Patients should be informed that when the medication is reduced and stopped, the likelihood of a transient rebound or persisting insomnia exists and this is not an indication to continue the hypnotic. If a benzodiazepine needs to be continued for a longer period of time it is advisable for the patient to take drug free intervals wherever possible. Studies do not support the long-term use of benzodiazepines. A careful tapering regime should be followed when stopping hypnotics for those with hypnotic dependency to avoid withdrawal reactions, as well as referring the patient for addiction counselling.3
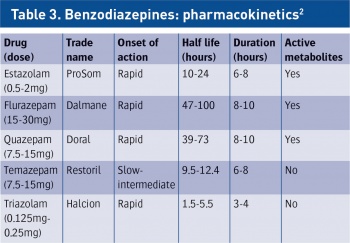
When deciding which benzodiazepine to choose, the main difference between them lies in their half life. Table 3 outlines the pharmacokinetic profile of commonly used benzodiazepines. Longer half lives can cause possible ‘hangover effects’ or amnesia in the morning, as seen with flurazepam, due to sedation which persists beyond the desired seven to eight hours of sleep time and impacts on waking function.
It is important to match the sedative hypnotic with the type of difficulty the patient is experiencing. For patients with difficulty initiating sleep, a short or intermediate-acting benzodiazepine is recommended. Intermediate-acting benzodiazepines are also recommended for patients who have early morning awakening or wake during the night. If patients wake during the night they should be advised not to take hypnotics as this reinforces awakenings. In general, long acting hypnotics should be avoided to ensure there is no sedative hangover during the day.2,3
Long term benzodiazepine use can lead to tolerance, drug dependency, benzodiazepine withdrawal syndrome upon discontinuation and long-term worsening of sleep. Sedative hypnotics should be used with extreme caution in the older population given the frequency of polypharmacy and drug interactions as well as delayed metabolism effects, falls risk and worsening of cognitive function. They should also be used with caution in patients with alcohol dependency, obstructive sleep apnoea and in those with renal, liver and respiratory disease.7
Non-benzodiazepine hypnotics
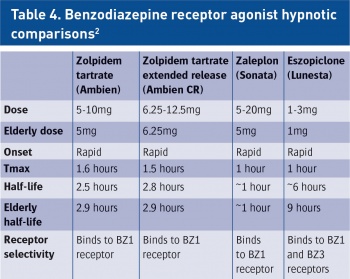
The newer non-benzodiazepine sedative-hypnotic drugs are similar to benzodiazepines in their mechanism of action and are indicated for mild to moderate insomnia. They are also known as the ‘Z drugs’ and include zolpidem, zaleplon, zopiclone and eszopiclone. Table 4 outlines the comparisons among these medications. Similar to the benzodiazepines the decision which agent to choose depends on the half life. In general, they are preferable to the more traditional benzodiazepines as they have less or no disruption to sleep architecture compared to the benzodiazepines and have much fewer adverse effects including daytime sedation, cognitive impairment, dependence and rebound insomnia.2,3,7
Zolpidem extended release (Ambien CR) is a combination of immediate release and modified-release components used to achieve initial plasma levels and peak concentrations, while maintaining higher levels for a longer period, extending the duration of efficacy. This allowed zolpidem ER to be approved for treatment of both sleep initiation and sleep maintenance difficulties.2
Other medications
There are many other prescribed agents in use but not licensed as hypnotics. Low doses of sedative antidepressants are commonly used but are poorly supported by research data and carry considerable side-effect profiles. The use of trazodone and other sedating antidepressants (including TCAs such as amitriptyline and doxepin) to promote sleep is based on the sedative effects of these agents rather than on demonstrated sleep promoting properties. Their use is of limited benefit unless the patient is suffering from depression. Several studies however have shown that trazodone is effective in treating insomnia for patients on SSRIs or SNRIs.2
Atypical antipsychotics including quetiapine and olanzapine are sometimes used off-label to treat insomnia. There is little evidence to support this and there is a significant risk of adverse effects associated with their use, particularly in the elderly population. Doses remain uncertain for the treatment of insomnia since there are no published studies demonstrating the effectiveness of these agents in patients with sleep disturbance.2
Melatonin is a hormone secreted from the pineal gland in darkness in order to control the sleep cycle. Ramelteon, a melatonin receptor agonist increases sleep time due to a melatonin rhythm shift with no evidence of next day residual effects. Melatonin was licensed for use in Ireland in 2009 at a 2mg dose for short-term treatment of primary insomnia in patients over 55-years-old.3,7
Over the counter insomnia treatments
Many patients choose OTC sleep aids as they are low cost, readily available options that are perceived as safe. Sedating antihistamines (eg. hydroxyzine and diphenhydramine) are commonly used. The effectiveness of antihistamines for sleep may worsen over time and patients can develop anticholinergic side effects. Their use is not recommended beyond a limited term due to daytime sedation, reduced cognitive function, drug interactions and the development of tolerance.
Valerian is a herbal extract that is available as an OTC hypnotic. The Irish Sleep Society do not recommend this medication as there is no robust data supporting its hypnotic effect and safety. Case reports of paradoxical reactions and hepatotoxicity have been described.3

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)