CANCER
Misinformation: a modifiable risk factor for cancer
Dispelling myths and misunderstandings about the causes of cancer is key to reducing prevalence
November 1, 2012
-
Many people in Ireland, including health professionals, are highly misinformed about the important role lifestyle factors play in raising their risk of developing cancer. Worryingly, nearly one in five people believe that their lifetime risk of cancer is non-modifiable.
That’s according to the results of a survey by University College Cork (UCC), presented at the European Society for Medical Oncology (ESMO) 2012 Congress in Vienna recently, which highlighted the significant challenges of overcoming myths and misunderstandings about cancer risks.
Understanding cancer risk
Commenting on the research, Dr Derek Power, medical oncologist at Mercy and Cork University Hospitals, and one of the lead authors of the study, said a large proportion of people overestimate the cancer risk attributable to genetics, yet underestimate the cancer risks associated with obesity, alcohol and sunlight exposure.
“Many myths surrounding cancer risk are also still popular,” said Dr Power. “For example, many people wrongly think that a blow to the breast, stress, wearing tight underwear, the use of mobile phones, genetically modified foods and aerosols are major cancer risk factors.”
Indeed, the survey found that almost 30% of respondents believe wearing a tight bra increases breast cancer risk and 48% are convinced that a blow to the breast does the same.
Lack of knowledge of cancer risk
While most people are aware of the classic risk factors, such as smoking and poor diet, a significant number appear misinformed about several proven cancer risks.
Only about a third of people (32% of the public and 41% of healthcare professionals [HCPs]) realised that obesity is a cancer risk factor, despite warnings from the World Health Organization that up to 41% of certain cancer burdens are attributable to overweight and obesity. Also, 33% of the public and 24% of HCPs did not think the location of fat was important.
“We didn’t set out to specifically look at healthcare professionals’ awareness of cancer risks but when we broke down the survey data the figures were very similar between what the general public and healthcare professionals believed,” said Dr Aoife Ryan, a lecturer in nutritional science at UCC and one of the lead authors of the research.
“The results are astonishing; basically, a large portion of the Irish population is misinformed and unaware of the real risk factors for cancer.”
The research, which is the first of its kind in Ireland, was conducted as a final-year thesis by UCC nutritional science undergraduates Lisa Burns and Ursula Kenny, under the guidance of Dr Ryan and Dr Power, and in association with Breakthrough Cancer Research and the Irish Cancer Society.
“Lisa and Ursula constructed a 48-question survey themselves because there was nothing like this done in Ireland before and only one or two similar studies published in the US,” Dr Ryan added.
“There was a tremendous response to the survey – 748 people replied. Most of them were women, only 100 men contributed. About 40 or so people declared that they had cancer and 126 (17%) said they were healthcare professionals.”
Barriers to prevention
The researchers were concerned to find that almost one in five people incorrectly believe that they can do nothing personally to prevent cancer if they have a family history of the disease.
“Overall, 90% of respondents, including healthcare professionals, believed genetics ‘strongly’ increases risk,” said Dr Power.
“More than one in four of the public believed that over 50% of cancers are genetic. Incredibly, 15% of people we surveyed believed lifetime risk of cancer is non-modifiable.
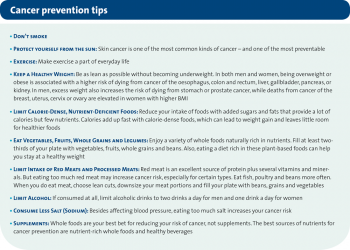
“This misinformation needs to be addressed in health promotion campaigns, emphasising that diet and lifestyle, including smoking, account for 90-95% of cancers,” he stressed. “Only about 5-8% of cancers, depending on cancer site, are due to an inherited gene.”
Stress, as a cancer trigger, was another major misconception, said Dr Ryan. “Ninety-two percent of people thought stress was a risk factor, in contrast to scientific evidence that shows this is not a risk factor. There are some interesting data from the National Cancer Institute in the US that stress can shorten your lifespan once you have cancer. It’s very hard to study whether stress causes cancer but most people think that it does.
Diet and nutrition myths
“We also found that more than about 50% of those surveyed believe that taking vitamin and mineral supplements can protect you against cancer, and about 20% thought they should be consumed daily, in contrary to the evidence that suggests we should not be taking them. In fact, high doses of vitamins and minerals can actually increase your risk of certain cancers, especially if you are a smoker,” she cautioned.
“This ties in with another myth held by one in five people that nutritional needs cannot be met by diet alone and supplements are absolutely necessary. The majority also believe that detox diets and organic food reduces cancer risk – again there is no evidence to support this.
“I was surprised to find that a large percentage of people didn’t know that frozen vegetables and fruit are every bit as good as fresh. A high number were also not aware that red meat is a risk factor or that salt can increase cancer risk.
“And it seems the red wine message is getting a bit confused: in moderation it may have some cardioprotective effects but about four in 10 people think it can protect against cancer too. Alcohol, any type of alcohol, is associated with an increased risk of a number of cancers. The advice would be to limit alcohol. If consumed at all, limit to two drinks for men and one for women per day,” Dr Ryan advised.
Obesity and cancer
A crucial public health message that appears to be missing its mark is that excess pounds do more than increase weight – they increase the risk of cancer, as well as a myriad of other health problems.
In both men and women, being overweight or obese is associated with a higher risk of dying from cancer of the oesophagus, colon and rectum, liver, gallbladder, pancreas or kidney.
In men, excess weight also increases the risk of dying from stomach or prostate cancer.
And deaths from cancer of the breast, uterus, cervix or ovary are elevated in women with higher body mass index (BMI).
Yet, in the UCC survey, only two in five healthcare professionals and a third of the public are aware of this risk.
“Obesity is a well known risk factor for many cancers. In some cancers, over half of them are thought to be directly caused by obesity,” said Dr Ryan.
Location of body fat
“We also found that a high number of people, including healthcare professionals, did not know about the correlation between cancer and the location of fat in the body. For certain cancers, such as colorectal cancer, it’s not just BMI, it seems to be fat on the waist that increases risk. So, visceral fat – deep-lying fat in the abdomen – is very metabolically active, secreting a whole host of substances that are implicated in cancer growth,” she explains.
“We published a number of research papers, when I worked in St James’s Hospital in Dublin with Prof John Reynolds, looking at obesity and cancer. We found that being overweight increased the risk of oesophageal cancer 11-fold in Irish people. We also found that a person with cancer who is obese is worse off. In a number of cancers we found that obese patients have on average 2cm bigger tumours and have more lymph nodes and vascular invasion than thinner people.
“What struck those of us involved in the UCC research is that this is a very well educated population, in fact it may even be biased in that they are too well educated; 52% of then had a college degree and one in five had a postgraduate degree, even though we deliberately did not send out the survey through the university. We tried to get a sample of the general public but we obviously got an educated sample, and even still there was a surprising amount of old wives’ tales and misinformation about cancer risks.”
Lifestyle choices do make a difference
Dr Power voiced the research team’s aspiration that, by sharing these common misunderstandings and informing the public about proven cancer risks and preventable measures, they can help people to make lifestyle choices that will reduce their risk of developing the disease.
“This will ultimately help to decrease the growing statistics of those diagnosed with cancer in Ireland,” he added.
With up to 41% of certain cancer burdens attributable to overweight and obesity, the study authors maintain that it is vital to raise awareness of obesity and physical inactivity as risk factors. However, it seems that as a nation we are in denial about our expanding waistlines.
Despite the fact that two-thirds of the Irish population is either overweight or obese, recent research by Safefood – the all-island food safety promotion agency – found that only 40% of people acknowledge that they have a weight problem.
 (click to enlarge)
(click to enlarge)
