RESPIRATORY
New GOLD standard in COPD guidelines
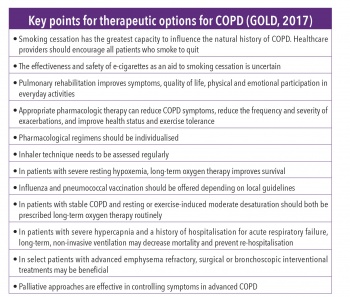
Recent updates to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines and their implication for clinical practice
February 8, 2018
-
In late 2016, the Global Initiative for Chronic Obstructive Lung Disease guidelines were updated.1 This article addresses the changes in these guidelines and the implication for clinical practice.
Definition of COPD
The definition of COPD has been revised to recognise the importance of precipitating factors. ‘COPD is a common, preventable and treatable disease that is characterised by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases. The chronic airflow limitation that is characteristic of COPD is caused by a mixture of small airways disease (eg. obstructive bronchiolitis) and parenchymal destruction (emphysema), the relative contributions of which vary from person to person”.1,2
The risk of developing COPD is related to tobacco smoke, indoor air pollution, occupational exposures, outdoor air pollution, genetic factors, age and gender, lung growth and development, socioeconomic status, asthma and airway hyper-reactivity, chronic bronchitis and infections.
ABCD assessment tool
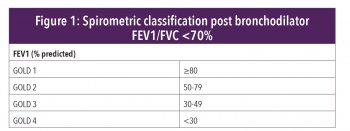
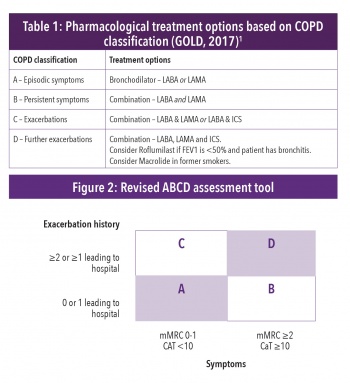
The assessment of COPD has been refined to include assessment of symptoms and risk of future exacerbations. With the original assessment tool, it was sometimes difficult to classify patients as some patients fell into more than one group. The spirometric assessment has been removed from the assessment tool which has simplified the classification. However, spirometry is still required for confirmation of diagnosis and to assess severity of airflow limitation (Figure 1). Spirometric assessment is based on post-bronchodilator FEV1/FVC ratio less than 70%.
To assess symptoms, two assessment tools are used – the Medical Research Council Scale and the COPD Assessment Test. Exacerbation history is based on the number of exacerbations in the previous 12 months. Figure 2 illustrates the revised ABCD classification. The revised tool provides a more individualised approach to patient assessment and management.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)