CANCER
Non-Hodgkin lymphoma survivorship in Ireland
Survivorship rates for non-Hodgkin lymphoma in Ireland
August 9, 2016
-
Approximately 700 Irish people are diagnosed with non-Hodgkin lymphoma (NHL) each year.1 Furthermore, the number of new cases is increasing by about 3-5% annually,2 and it is estimated that it will be as common as breast or lung cancer by 2025.3 This increase can be partly attributed to our ageing population, with 66 being the median age of diagnosis in Ireland.1 However, in recent years, NHL mortality rates have begun to stabilise. This suggests that the prognosis for NHL patients in Ireland has improved, which is reflected in the increased survival rates. According to recent figures from the National Cancer Registry of Ireland, five-year relative survival has increased from 47.3% in 1994 to 64.1% in 2012.1 As a result, there are now more NHL survivors in Ireland than ever before.
NHL survivors
The National Cancer Institute considers a person to be a cancer survivor “from the time of diagnosis until the end of life”. Although the growing number of survivors is a welcome sign of progress, this trend also presents a challenge because many of these individuals require significant, ongoing care, such as surveillance for cancer recurrence, screening for new cancers, and care for the long-term effects of their initial treatment. As a result, survivorship should now be seen as a new diagnosis, as well as a new medical speciality in its own right.
Six-in-10 patients who either present with, or transform from an indolent to an aggressive form of NHL (eg. follicular lymphoma → diffuse large B cell lymphoma) can be cured with intense protocols, such as multi-agent chemotherapy as well as additional radiotherapy and, potentially, bone marrow/stem cell transplantation. These aggressive forms tend to have a short natural history, with the greatest risk of relapse being within two years of ending treatment.4 However, survivors can be left with long-lasting side-effects such as cardiac dysfunction, cognitive impairment, secondary comorbidities and sexual dysfunction, as well as psychosocial sequelae.
Furthermore, it has been reported that cancer survivors are almost twice as likely to have at least one functional limitation.5 These late effects may adversely impact survivors’ health-related quality of life (HRQoL), a multidimensional concept including domains relating to patient physical, mental, emotional and social functioning which has become synonymous with cancer survivorship in recent times.
Multi-level impact
The impact of a NHL diagnosis on the physical health of the survivor is reported on in various forms of literature. A study by Smith et al,6 found that those with active NHL disease had poorer physical functioning and QoL than disease-free survivors. Mols et al7 found that NHL survivors exhibited significantly lower scores than the normal population for general health perception (GHP)
(P < .001) and vitality (P < .001).Furthermore, the psychological impact of diagnosis can result in negative health outcomes for the survivor. Most NHL survivors have undergone chemotherapy, radiotherapy, or a combination of both as part of their treatment. Survivors who have received chemotherapy or who currently had active disease described significantly poorer psychological and social wellbeing and QoL than those who had not.8
This can also be seen in a cross sectional exploratory study conducted by Smith et al in 20119 in which it was found that one of the strongest QoL relationships (P < .001) was for post-traumatic stress disorder-like symptoms found in survivors, which were as a result of their diagnosis. It is therefore very clear to see the detrimental impact a cancer diagnosis can have on an individual’s psychological wellbeing and their ability to cope during such an uncertain and stressful time. As well as this, the obvious financial burden associated NHL has been widely reported in many studies,7,10 in which it has been found that those survivors earning less than a certain income bracket have a poorer QoL outcome.
The Functional Assessment of Cancer Therapy – General (FACT-G) is a standardised, validated, HRQoL measure. It has been used across the literature to demonstrate the effect of having one or more comorbidity coupled with NHL. One such study,11 found that for every point increase in comorbidity score, the FACT-G score was 1.35 points lower. A study conducted by Smith et al in 20096 found that 60% of NHL survivors were either unemployed or retired due to issues related to their condition.
Furthermore, Mols et al7 reported that 41% of survivors indicated that they had changed jobs, reduced working hours or stopped working entirely as a result of their cancer. Other related studies have also found that NHL survivors who were employed reported a higher QoL than those who didn’t, which demonstrates the added benefit of employment to functional wellbeing.9,11 Functional change at any point in the survivorship trajectory may require changes to housing arrangements as well as the amount of support provided. This QoL domain has gained more attention as the population continues to age in order to accommodate these associated effects on daily living.
QoL research in Ireland
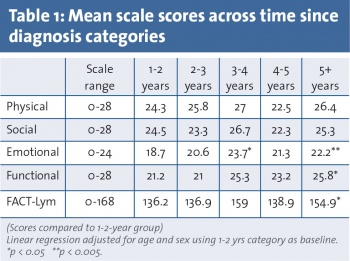
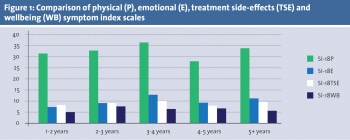
As the number of NHL survivors in Ireland increases, there is a growing need for research focused on quality of life (QoL) outcomes in this population. Our research set about assessing the QoL in an Irish population of non-Hodgkin lymphoma (NHL) survivors. High-grade NHL survivors treated in two university hospitals participated in this cross-sectional study by completing the validated Lymphoma-specific Functional Assessment of Cancer Therapy (FACT-Lym) questionnaire, and the National Comprehensive Cancer Network-Functional Assessment of Cancer Therapy Lymphoma Symptom Index-18 (FLymSI-18). The FACT-Lym is centred around the aforementioned generic core questionnaire, the FACT-G. This is a compilation of general questions divided into the four primary QoL domains: physical, social, emotional, and functional well-being. It is considered appropriate for use with patients with any form of cancer, and has also been used and validated in the general population. Our population scored a mean of 94 out of a range of 58-108, with a SD of 13. With regards to lymphoma-specific QoL, this population scored a mean of 60 out of a range of 33-72, with an SD of 10.4 (see Table 1).
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)