LEGAL/ETHICS
WOMEN’S HEALTH
Protection of Life during Pregnancy Act guideline
An examination of the Department of Health’s guidance for health professionals on the Protection of Life during Pregnancy Act 2013
November 3, 2014
-
The Department of Health have issued its guidance on the Protection of Life during Pregnancy Act 2013. The ICGP Quick Reference Guide on Crisis Pregnancy has been updated to include an appendix that summarises the guidance, with a particular emphasis on the roles and responsibilities of GPs as envisaged in the guidance.
The Protection of Life during Pregnancy Act, enacted in July 2013 and commenced in January 2014, was Ireland’s response to a European Court of Human Rights judgement that put an obligation on the State to put a legal framework in place to allow a pregnant woman to test her entitlement as to whether she qualifies for a lawful abortion in Ireland on grounds of the risk to her life because of her pregnancy. The guidance is designed to assist health professionals in operating the Act when providing care to pregnant women with life-threatening conditions. The Department of Health states that they are not clinical guidelines.
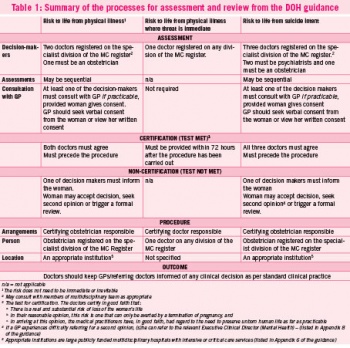
The Act and the guidance describe complex requirements for the assessment and certification of a woman presenting in such circumstances with either one, two or three doctors involved. If the doctors undertaking the assessment judge that the woman does not meet the test for certification then she (or someone on her behalf) can apply for a review of her case, and again the requirements for carrying out the review are complex.
With the exception of an imminent threat to the woman’s life, an abortion certified under this Act can only be carried out in an ‘appropriate institution’. These are listed in an appendix to the guidance.
The likely involvement of GPs is specified in three areas:
- Referral
- Providing clinical information to the assessment panel (subject to the woman’s consent)
- Providing information to the review panel.
Referral pathways are described for physical and psychiatric risks. One of the doctors on the assessment panel must consult the GP ‘if practicable’, only if the woman consents. A GP is advised to seek verbal consent from the woman to provide information or see her written consent. There is a statutory duty on doctors (including GPs) to provide documents or appear before the review panel, if requested to do so. The framework is summarised in Table 1.
Potential difficulties with the Act have been described by Doran and Cronin (Forum, November 2013), including a lack of transparency about the selection of ‘appropriate institutions’, the absence of an opt-out clause for hospitals and the absence of procedural clarity in organising reviews. These issues have not been expanded upon significantly in the guidance.
In its submission on the legislation, the ICGP (as reported in Forum, July 2013) expressed concerns about confidentiality, a referral pathway and the lack of detail on the nature of the consultation by the deciding doctors with the woman’s GP. These concerns have been addressed in part in the guidance document. There is some general guidance about confidentiality but the specific concerns of the ICGP have not been addressed. Referral pathways have been outlined, although the availability of the psychiatric referral pathway in particular has yet to be tested throughout the country. There is no further detail in the guidance as to the nature of the consultation of either the assessment panel or a review panel with the woman’s GP.
Reaction to the guidance in the general media has been mixed, with reservations being expressed by organisations from across the pro-life/pro-choice spectrum. The purpose of the Act (and the related guidance) is to provide a procedure by which a woman can establish whether she qualifies for a lawful abortion in Ireland on grounds of the risk to her life as a result of her pregnancy. The complexity of the structures for referral, assessment and review in circumstances where time is critical puts onerous responsibilities on the woman, her GP and the large number of doctors who can be involved. The degree of urgency and co-ordination required in the appropriate institutions and the HSE will also be very challenging.
Some commentators are of the view that this very complexity indicates the inherent difficulty with the wording of the 1983 amendment, and they argue that the country may need to revisit the Constitution.
 (click to enlarge)
(click to enlarge)
