DIABETES
Screening for AF in diabetes patients
With diabetes patients at a higher risk of atrial fibrillation than the general population, there is a case for introducing routine screening for AF
April 1, 2015
-
Atrial fibrillation (AF) is the most common form of arrhythmia, with a prevalence of 0.1% among adults younger than 55 years, rising to 9% in people aged 80 years or older. As the world’s population ages, it is estimated that the prevalence of AF will increase two-and-a-half-fold in the next 50 years.1
AF is associated with an increased risk of stroke, congestive heart failure, cognitive dysfunction, reduced quality of life and increased all-cause mortality. The mortality rate of people with AF is almost twice that of the ordinary population for several reasons, including the fact that AF results in an approximate three- to five-fold excess risk of stroke.2 Also, the number of strokes associated with AF dramatically increases with age, from 1.5% for those 50 to 59 years of age to 23.5% for those 80 to 89 years of age.3
Stroke due to AF is twice as likely to result in greater functional impairment in those who survive, and is twice as likely to be fatal compared to strokes in those without AF.4
Diabetes is known to increase a person’s risk for cardiovascular disease but may confer an excess risk of stroke that is independent of blood pressure.5
It is estimated that there are 191,380 people with diabetes in Ireland with a prevalence of 6.1% in the population, and that by 2030 there will be 278,850 people with the condition with a prevalence of 7.5% in the population.6
Population-based studies also suggest that diabetes is an independent risk factor for atrial fibrillation.7 What is more, sub-clinical episodes of AF are thought to occur more frequently in type 2 diabetes patients and these are associated with a significantly increased risk of silent cerebral infarcts and stroke.8
Therefore, the fact that AF and diabetes both significantly increase a person’s risk for stroke, combined with the increasing prevalence of both diseases, and the fact that diabetes is an independent risk factor for atrial fibrillation, led us to look at whether screening for AF should be undertaken in our type 2 diabetes population.
Screening for atrial fibrillation meets many of the Wilson-Jungnen criteria for screening for disease:
• The condition is an important health problem
• There is a suitable test for diagnosis
• There is accepted treatment for people following diagnosis
• The gold standard to detect atrial fibrillation is a 12-lead ECG interpreted by a cardiologist, however other tests that can be used may involve alternative types of ECG, ie. limb lead, 3-lead or 5-lead ECGs interpreted by a GP, with preliminary pulse palpation.
Aims of study
The aims of the study were to:
• Examine the prevalence of atrial fibrillation in our type 2 diabetes population
• Compare the actual prevalence with the already known cases
• Identify what percentage of newly discovered patients with atrial fibrillation needed further medical follow-up
• Determine if ECG examination should be a part of our diabetes review.
It should be noted that routine ECGs are currently not part of the NICE or ICGP diabetes guidelines for annual review.
Recruitment through diabetes clinic
Patient recruitment was undertaken through the diabetes clinic run in our practice. The purpose of the study was explained to our patients, and they were invited to participate in this research study involving a 3-lead ECG carried out by the practice nurse. Participants understood that the aim of the study was to pick up atrial fibrillation and was for research purposes only.
Every patient who participated signed a consent form and the practice nurse carried out a 3-lead ECG in the diabetes clinic on an opportunist basis.
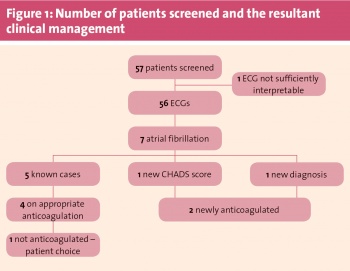
Study results (see Figure 1)
A 3-lead ECG was carried out on 57 patients. One ECG did not meet appropriate clinical interpretation standards and was discarded.
Of the 56 ECGs carried out, seven showed atrial fibrillation. On review of each patient’s clinical notes, five of these cases were already documented. Of the five known patients with atrial fibrillation, four were on appropriate anticoagulation.
One had declined warfarin as anti-coagulation because he was a missionary priest working in Africa and could not be properly monitored, with the other forms of oral anticoagulation not available to him.
Of those patients who were not on anti-coagulation, one patient had previously been documented as having paroxysmal AF, but on reviewing this patient’s clinical history – and the fact that he was now in persistent AF with a diagnosis of type 2 diabetes giving him an increased CHADS score –he was referred to cardiology with the intention of starting him on anticoagulation.
One patient was a newly diagnosed case of AF, and was also referred to cardiology for consideration of anticoagulation and cardioversion.
Therefore, in our study group the prevalence of AF in the type 2 diabetes population was approximately 12.5% (7/56). The incidence of unknown fibrillation in the same population was 1.8% (1/56). A total of 3.6% (2/56) of patients required further medical evaluation or investigation. Of note is that all the patients who were diagnosed with AF were aged 65 or older.
 (click to enlarge)
(click to enlarge)
