INFECTIOUS DISEASES
LEGAL/ETHICS
Screening for hepatitis C
New Irish guidelines on hepatitis C (HCV) highlight the need to identify and screen people with potential undiagnosed HCV infection
November 10, 2017
-
Hepatitis C virus (HCV) is a major cause of liver disease worldwide. Globally, it is estimated that there are 115 million people who have had HCV infection, and 80 million with chronic infection.
According to the HSE’s Health Protection Surveillance Centre (HPSC) there were 652 notifications of hepatitis C in 2016 (14.2/100,000 population). This is a small decrease compared to 2015 (n = 675, 14.7/100,000 population). Although the number of cases of hepatitis C reported has declined by 58% since peak levels in 2007 (n = 1,538), recent trends indicate that levels are stabilising rather than continuing to decrease, the HPSC says. HCV infection has been a notifiable disease in Ireland since 2004. Between 2004 and 2016, 14,107 cases were notified.
National guidelines
According to recently produced Irish guidelines on HCV screening,1 injecting drug use (IDU) is the major risk factor for HCV in developed countries such as Ireland. Initial infection with HCV is typically asymptomatic or mildly symptomatic. The most common symptoms are loss of appetite, abdominal discomfort, nausea/vomiting, and jaundice. Infection is rarely detected in the acute phase. Between 15%-45% of those infected clear the virus spontaneously, while the remaining 55%-85% of those infected develop chronic HCV infection.
Chronic HCV infection can cause liver inflammation, fibrosis, cirrhosis, liver cancer, liver failure and death. Chronic liver disease symptoms may not be evident for 20 to 30 years until serious liver damage has occurred. For this reason, the guidelines point out, HCV infection is sometimes called ‘the silent killer’.
Progression to chronic liver disease is associated with excessive alcohol intake, co-infection with hepatitis B virus (HBV) or human immunodeficiency virus (HIV), being male, and older age.
The new guidelines note that advancements in treatment for HCV infection that offer a cure in most cases, and are more acceptable to patients, have led to a significant shift in strategy direction for HCV care and policy, with the paradigm now focused towards elimination.
Where risk factor data are available, IDU is the most common HCV risk factor reported (80%), followed by possible sexual exposure (5%), receipt of blood or blood products (4%), vertical transmission (2%) and tattooing or body piercing (1%). In 7% no risk factor was identified.
Notification data can only include diagnosed cases. Information on the prevalence of a disease is a better reflection of the burden of disease as it includes undiagnosed cases. It is estimated that there are between 20,100 and 42,000 people with current infection in Ireland, and that 60% of those have not yet been diagnosed.
Hospital admissions
The number of hospital admissions due to end-stage liver disease (ESLD) and hepatocellular carcinoma (HCC) in those with HCV infection has been increasing in Ireland. This increase is likely related to the fact that the peak incidence in the largest risk group, people who inject drugs (PWID) in Ireland, was in the late 1990s, and those infected during that period are now developing end-stage liver disease or hepatocellular carcinoma (HCC). Between 2005 and 2016, 116 liver transplants were performed in Ireland in people with HCV infection, accounting for 18% of all liver transplants.
Direct-acting antiviral (DAA) therapies are now the standard of care for HCV infection, according to the guidelines. In HCV treatment, sustained virological response (SVR) means that the virus is no longer detectable at a defined period after completion of therapy. SVR is regarded as a virological cure and is associated with improved morbidity and mortality. Older treatment regimes induced SVR rates of 40-65%. DAA treatment regimes are of shorter duration, with far fewer side effects, and have SVR rates of over 90%. Further details on the new treatments are available at www.hse.ie/eng/health/az/H/Hepatitis-C/
It is now recommended that DAA regimens be used for the treatment of persons with HCV infection. In order to ensure the most appropriate management of access to these costly new drugs, an Expert Advisory Group was established by the Department of Health (DoH) in 2014, which recommended the establishment of the National Hepatits C Treatment Programme (NHCTP) in the HSE.
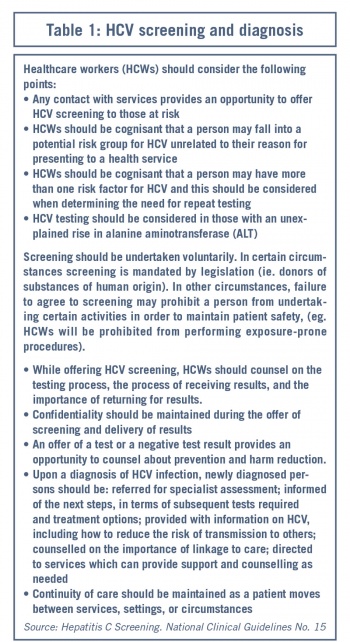 (click to enlarge)
(click to enlarge)
