RESPIRATORY
Stepwise approach to asthma: latest thinking
The essence of asthma management is proper diagnosis, assessment and regular review
March 3, 2014
-
Asthma is a major cause of chronic morbidity and mortality throughout the world and there is evidence that its prevalence has increased considerably over the past 20 years, especially in children.1 This increase has been paralleled in other atopic and allergic disorders suggesting the increase is systemic rather than confined to the lung.2
Asthma is a chronic inflammatory disorder of the airways. Chronically inflamed airways are hyper-responsive; they become obstructed and airflow is limited (by bronchoconstriction, mucous plugs and increased inflammation) when airways are exposed to various risk factors. Many cellular components are involved in the asthmatic pathway, including mast cells, eosinophils, T-lymphocytes, macrophages, neutrophils and epithelial cells.3
The key approaches to asthma are both graduated medication treatment and an optimal lifestyle approach such as smoking avoidance/cessation and avoidance of environmental triggers. Medicinal treatment tends to be divided into both preventative and relieving categories. In optimal control the requirement for relieving medication is kept to a minimum.
This article summarises the key latest guidelines. The main guidelines referenced are the latest GINA guidelines1 and the SIGN guidelines of the British Thoracic Society.2 Asthma as a single disease entity accounts for 1-2% of a nation’s total health budget, the importance of adequate control and a structured preventative approach cannot be understated.
Prevalence
Asthma is one of the most common chronic diseases globally and currently affects approximately 300 million people. The incidence in adults is 10‑12%, and 15% of children are affected by the disease.2 Healthcare data from the US show that, annually, those affected by asthma are hospitalised nearly 500,000 times with two million emergency department visits, 100 million sick days accumulated and 5,000 deaths. Rates of hospitalisation are highest among black people and children, with deaths highest among black youths from 15-24 years of age.4 Ireland has one of the highest prevalences of asthma in the world, fortunately the mortality rate compares more favourably.5
Aetiology
Asthma is a complex disease with underlying multi-gene association interacting with environmental exposure. Patients’ genetic make-up may predispose them to hyper-responsiveness to environmental aetiological triggers. Those triggers include:
- Viral infections, eg. rhinovirus, respiratory syncytial virus, human metapneumovirus and influenza virus
- Bacterial infections – Mycoplasma pneumoniae or Chlamydia pneumoniae
- Allergen exposure, eg. tree, grass or weed pollen; fungi; or indoor allergens
- Occupational exposures, eg. animal or chemical
- Food additives and chemicals, for example, metabisulfites, irritants or aspirin in predisposed people.
Clinical features
The key typical clinical features of asthma include recurring episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning.6
Classification/severity
Of note, the classification may change over time depending on the patient’s health status. One factor in each category is sufficient to classify a patient. Asthma is a variable disease, thus there can be overlap between categories.3 The classification of asthma is pivotal to our level of urgency and the level of intervention we institute.
Mild intermittent
- Symptoms ≤ 2 times a week
- Asymptomatic and normal peak expiratory flow rate (PEFR) between attacks
- Attacks are brief with varying intensity
- Night-time symptoms ≤ 2 times a month
- Forced expiratory flow at 1 second (FEV1) or PEFR ≥ 80% of predicted
- PEFR variability < 20%.
Mild persistent
- Symptoms > 2 times a week but < 1 time a day
- Exacerbations may affect activity
- Night-time symptoms > 2 times a month
- FEV1 ≥ 80% of predicted
- PEFR variability between 20% and 30%.
Moderate persistent
- Daily symptoms
- Use of short-acting beta agonists daily
- Attacks affect activity
- Exacerbations ≥ 2 times a week, may last for days
- Night-time symptoms > 1 time a week
- FEV1 greater than 60% to < 80% of predicted
- PEFR variability > 30%.
Severe persistent
- Continual symptoms
- Limited physical activity
- Frequent exacerbations
- Frequent night-time symptoms
- FEV1 ≤ 60% of predicted
- PEFR variability > 60%.
Management
The approach to asthma management is stepwise, encompassing regular review and adaptation to current symptoms. The most recent GINA guidelines advised incorporating four inter-related components of therapy to achieve and maintain control of asthma.1
- Component 1: develop patient/doctor partnership for a collaborative approach
- Component 2: identify and reduce exposure to risk factors
- Component 3: assess, treat and monitor asthma
- Component 4: manage asthma exacerbations.
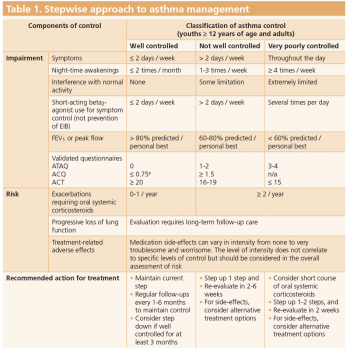
The management of asthma is classified by whether it is controlled, poorly controlled or uncontrolled. This approach is summarised in Table 1.
This guided approach enables us to subdivide the assessment into these key groups, which can then form the framework for the management approach. For simplicity and brevity we will restrict the management approach to children older than five years, adolescents and adults. We must ensure that the patient’s inhaler technique and compliance are optimal before we make any recommendations on their control.
Fortunately, the guidelines have structured the approach formatted in a simple step-up, step-down approach. The change is structured on the basis of ongoing symptoms, limitation of activity and frequency of reliever use. Peak flow or spirometry readings can also be used where accessible. It is worthwhile noting that any acute exacerbation should initiate a review of preventative treatment.1 The treatment steps have five treatment steps, the last two incorporating lesser-used medications such as sustained-release theophylline and anti-IgE treatment. The anti-IgE is proven to be effective grade A evidence, although it is mediated by a specialist and cost can be a real-life deterrent.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)