INFECTIOUS DISEASES
Tackling a silent killer through screening
Given the availability of drugs that can effectively cure HCV infection, a renewed effort is required to identify the 60% of undiagnosed people in Ireland
January 5, 2018
-
Hepatitis C virus (HCV) is a major cause of liver disease worldwide. Globally, an estimated 80 million people have chronic HCV infection.1 In Ireland there are between 20,100 and 42,000 people with HCV infection, 60% of whom are as yet undiagnosed.2,3,4 Between 55-85% of people infected go on to develop chronic infection, and between 15%-30% of those will develop cirrhosis, approximately 20 years after infection.1 HCV infection is sometimes called the ‘silent killer’ because symptoms usually don’t develop until liver disease is already advanced. It is also called silent because many of those infected or most at risk of infection are marginalised in society.
In recent years there have been major advancements in the treatment of HCV. Treatment with direct-acting antiretrovirals (DAAs) is now the standard of care.1,5 DAAs are highly effective, and are associated with virological cure rates of over 90%. Access to treatment in Ireland has been introduced through the HSE National Hepatitis C Treatment Programme (NHCTP) on a phased basis based on clinical criteria, with those having greatest clinical need receiving treatment initially.
Criteria for access to treatment are continually expanding. The NHCTP is aiming to provide treatment across a range of healthcare settings to all persons living with HCV in Ireland over the coming years.6 To date, since 2015 just over 2,000 people have been provided with treatment as part of the national programme. The availability of drugs that can effectively cure HCV means that screening for HCV is now more important than ever.
Globally, the availability of DAAs has shifted the focus towards elimination of HCV. In 2016 the World Health Organization (WHO) set a goal of eliminating viral hepatitis as a major public health threat by 2030.7 WHO has stated that national testing policies are needed, as are increased investments in HCV screening services, so that the goal of elimination can be reached.
Screening in Ireland
In Ireland, screening for HCV infection takes place in many settings, including in general practice. However, until now national guidelines on who should be screened and in what settings this should happen were not available. The need for national screening guidelines was recognised by the National Hepatitis C Strategy8 and, in response to their recommendation, a National Clinical Guideline on Hepatitis C Screening was developed to make recommendations on who should be screened for HCV and how that screening should be done.9 The guideline was developed under the auspices of the National Clinical Effectiveness Committee (NCEC). The NCEC was established by the Department of Health to support evidence-based practice.10
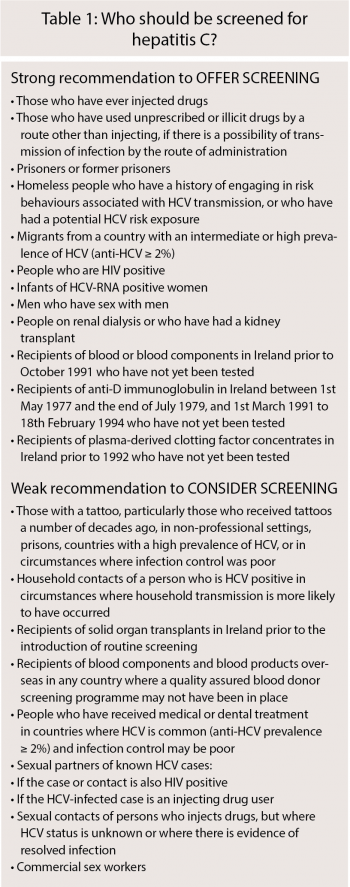
Box 1 summarises risk groups for whom screening is recommended by the new guidelines. The strength of recommendation reflects the confidence that the desirable effects of screening outweigh the potential undesirable effects. Where the evidence of the risk of HCV infection is clear and/ or the benefit of offering screening is considered high, a strong recommendation to offer screening has been made. When the evidence on the risk of HCV infection and/or potential benefit of screening is less clear, a weak or conditional recommendation has been made, which means that screening should be considered in these groups.
For many risk groups screening is already offered through dedicated health services (eg. addiction services, maternity services, occupational health services), as well as in general practice. For other risk groups the main, or in some cases only, healthcare contact, and therefore opportunity to be offered screening, will be their GP.
The recommendations for screening of some of the risk groups most likely to be encountered in general practice are discussed further here. The full suite of recommendations, along with the supporting evidence and rationale behind the recommendation, can be viewed in the National Clinical Guideline, or the summary version, which is available at health.gov.ie9
 (click to enlarge)
(click to enlarge)
