NEUROLOGY
Taking concussion in sport seriously
A structured approach will help doctors in the diagnosis and management of concussion
March 2, 2015
-
There has been extensive coverage about concussion in the media in recent times. This is in part due to the evolving knowledge base surrounding concussion and also due to the number of high-profile concussions in contact sport, such as that of Irish rugby player Jonathan Sexton.
A number of developments in Irish sport such as the faster pace of games, increased and more intense tackling, and the ‘bulking up’ of players pose a challenge for sporting organisations, schools and players alike.1 The consequences of recurrent concussive injuries are a topic of ongoing debate. Of note, there is currently a class action lawsuit against the National Football League (NFL) in the US, regarding concussion-related brain injuries. The value of concussion education is being increasingly recognised, involving players themselves, coaches and back-room staff. The current message is simple: concussion must be taken seriously as if it is ignored it could lead to death.
So what role does the GP play in managing a concussion injury and assessing when a player is fit to return to play?
Challenges in practice
In general practice, concussion can present in a number of different settings. The doctor may be pitch-side at the time of injury or see the patient in an out-of-hours setting.
A more common occurrence is the player presenting to the practice after the injury has occurred. This can pose challenges due to the time lapse between the occurrence of the injury and the patient attending. As the scenario above mentions, the doctor may be faced with challenges on a number of different levels and may experience difficulties with advice around when it is appropriate to return to play and the criteria to use to judge this.
Disturbance in brain function
Concussion may be defined as a disturbance in brain function caused by a direct or indirect force to the head. It results in a variety of non-specific signs and/or symptoms (see Figure 1)4 and most often does not involve loss of consciousness. Concussion usually results in functional disturbances rather than structural injury to the brain, so standard structural neuroimaging typically does not detect post-concussion brain abnormalities.2
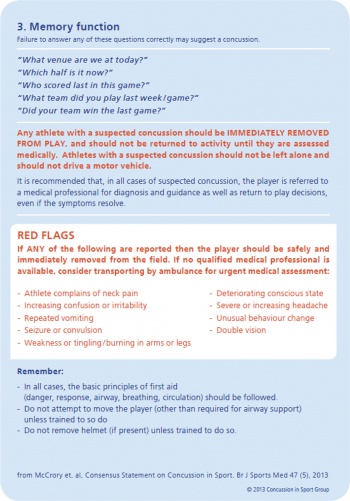
Concussion should be suspected in the presence of any one or more of the following:
- Symptoms (eg. headache)
- Physical signs (eg. unsteadiness)
- Impaired brain function (eg. confusion)
- Abnormal behaviour (eg. change in personality).3
The Zurich 2012 consensus statement on concussion reflects best practice in the management and treatment of concussion in sport.4
The statement urges: “Anyone suspected of suffering a concussion should be removed from play immediately and not return to play until they have been cleared by a medical practitioner. Questioning close relatives, especially parents or guardians in the case of children and adolescents, is often valuable. Any report that the individual ‘does not seem right’ or ‘is not themselves’ after trauma, is strongly suggestive of a concussive injury.”4
Return to play
The use of a graded symptom checklist can often be helpful.5 Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. Some 80-90% of concussions resolve in a short period (seven to 10 days), although the recovery timeframe may be longer in children and adolescents.
The current belief is that premature return to play and subsequent second injury before the athlete has fully recovered from the initial concussion may predispose to poorer outcomes.3 Adolescents are more vulnerable than both children and adults to the consequences of a sports concussion.6 The role of the GP is not only to assess the patient but also, in the case of young people, to educate their parents and carers about the risks concussion can pose.
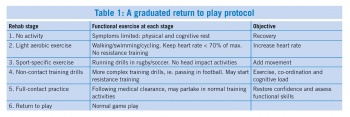
The GP should advise athletes that they should not return to play on the same day of the injury. For medical clearance to be given before return to play, the GP should follow a stepwise, symptom-limited programme, with stages of progression (see Table 1).3,4,5
Other important points:
- Rest and avoid strenuous activity for at least 24 hours
- No alcohol
- No sleeping tablets
- Use paracetamol or codeine for headache. Do not use aspirin or anti-inflammatory medication
- Do not drive, train or play sport until medically cleared.7
There should be at least 24 hours or longer for each stage, and if symptoms recur the athlete should rest until they resolve once again and then resume the programme at the previous asymptomatic stage.
If the athlete is symptomatic for more than 10 days, then consultation by a medical practitioner who is an expert in the management of concussion is recommended, with medical clearance before return to play.3
The Irish Rugby Football Union (IRFU) has introduced mandatory time out of the game for those with a suspected or confirmed concussion. Players at adult level must remain out for 21 days and players at underage level must remain out for 23 days. These times out of the game have been adopted by other rugby unions.7
Concussed athletes with a history of ≥ 3 concussions take longer to recover than athletes with one or no previous concussion.8
It can be concluded that repeat concussions could shorten a player’s career and may have some potential to result in permanent neurological impairment. This also adds weight to the need to individualise an athlete’s return to play and rehabilitation.
Take-home message
Any player with a concussion or suspected concussion should be removed from the field of play immediately and should not return to play, training or other physical activity on the same day. For medical clearance to be given before return to play, the GP should follow a stepwise symptom-limited programme, with stages of progression. GPs have an important role to play in educating players, trainers and families alike in concussion.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)