HEALTH SERVICES
The latest cut is the deepest
GPs believe the latest cuts confirm that the Government’s primary care plans are largely based on rhetoric and not on resourcing
September 1, 2013
-
Irish general practice has gone through dark times before – the periods prior to the introduction of the medical card scheme in the early 1970s and the ‘O’Connell deal’ in the early 1990s were fairly grim, before palliation arrived in the shape of Government initiatives.
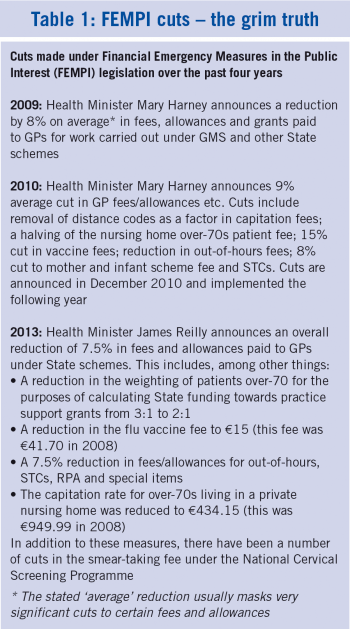
Now, an unprecedented level of gloom and doom is hanging over the specialty. GPs had in recent years carried on as best they could despite being battered by the effects of the recession and previous fee cuts under the Financial Emergency Measures in the Public Interest (FEMPI) legislation, and frustrated by the Government’s lip service and lack of resourcing for chronic care management in the community.
Many feel the latest FEMPI cuts (see Table 1) are the final straw.
The College’s decision to withdraw GP leads from clinical programmes, by no means taken lightly, was the most visible sign that the game is up as regards putting primary care at the centre of the health service.
The College feels that the Government’s primary care policy is more about rhetoric than resources. Members feel there is no bright new dawn ahead, just a ‘race to the bottom’. And worst of all, patients will suffer because of this neglect.
Sense of stagnation
Mel Bates, who is in practice in Dublin’s inner city, feels there is a real sense of general practice stagnating.
“It’s like being stuck on a stationary train waiting for it to move forward, but instead it goes backwards.
“The FEMPI fee reduction mechanism is a very blunt instrument in that it reduces fees for good initiatives as well as for some that may have seemed less value for money.
“GPs will just try to get on with the job whatever the circumstances, but practice resources will be affected – it may take patients longer to see their GP; the same range of services may not be provided.
“I would worry about overall morale being quite negative at the moment and about the effects of income reductions on younger doctors. Locally, I have not seen many recently trained GPs doing out-of-hour shifts and I would wonder what has happened to them. Certainly, the UK system is looking for GPs, and there they are better paid and better treated.”
Dr Bates feels it was a dark day for general practice and the Government when the College felt it had no alternative but to withdraw clinical leads from the programmes. “The fact that it had got to that stage in many ways typifies the attitude of the Government to general practice.”
No choice
A GP in a group practice in suburban Dublin, who did not wish to be named, told Forum that the net result of the FEMPI cuts on his practice, taking into account fixed overheads, was that his ‘take home pay’ from State work had reduced by 78% in recent years.
“Regretfully, we had no choice but to let go one of our assistants recently. We are seriously considering no longer doing flu vaccinations (the new E15 fee renders them unviable given the administrative work involved), we are thinking of stopping the on-call service we currently pay for and I am looking at the viability of continuing to provide nursing home cover in future.
“It is very uncomfortable to have to be so hard-headed about it. We already do a lot of pro-bono work, but given the financial straits we are in, we often feel we have no choice now but to concentrate as much as is feasible on the work that generates a reasonable income. Obviously, our patients are uppermost in our minds, but at the end of the day we are running a business and if a business is not generating enough income, then services inevitably suffer.”
As for taking on extra work such as care of additional diabetes patients, he said this was simply not a runner under the current circumstances.
Reduced level of service
Ray O’Connor, who is in practice in Co Limerick, says the latest FEMPI cuts will almost inevitably lead to a reduction in the level of service GPs are able to offer their patients.
“For example, I had a very positive 30 minute counselling session with a patient this morning. She could have walked out with a prescription after a consultation of less than 10 minutes, which would have been less satisfactory and more costly in terms of care provision. However, I really don’t know how much longer I will be able to provide that level of service.”
Ray O’Connor feels the latest fee cuts will threaten many GPs’ ability to provide optimal care for patients with chronic diseases.
As regards the Government’s plan to move additional diabetes patients from secondary to primary care, he says this is simply not financially viable without an injection of extra resources.
“At present, I have approximately 110 diabetes patients in my practice. We all agree that each patient should have at least an annual review focusing on their diabetes that is extra to any other clinical review.
“Doing this for all 110 patients averages nine per month over a full year – this is the minimum and many might need more frequent reviews. So if we go by the proposed HSE review schedule of four per annum then the cost would be E400 per patient per month. This level of resourcing would have to be provided as it is not available within the practice.”
Lack of resources
Midlands GP Dr Velma Harkins said while it was regrettable that the College felt it had no option but to withdraw from the clinical programmes, it was clear that all the pieces are not yet in place to transfer management of uncomplicated diabetes to the community.
She accepted that while the appointment of clinical nurse specialists as part of the programme was going ahead, the issue of practice resources to fully implement the new structure of care had still to be resolved.
While the new clinical nurse specialists would support the roll-out of the integrated diabetes care programme, these were not practice resources, Dr Harkins stressed.
Dr Tony O’Sullivan, who is in practice in south Dublin, says he totally agrees with the College’s decision to pull its representatives from the clinical programmes.
The diabetes programme in particular, he said, was the ‘great hope’ that would demonstrate how diabetes care could be successfully transferred from secondary to primary care, but this vision was now unlikely to be realised, due to the lack of resourcing for practices to take on the extra workload.
“Of course, many GPs are already providing this type of care, but in order to bring it onto the next level, proper resourcing was needed. If GPs were given the proper tools to do the job, they could have looked after things from there on in and provided optimal diabetes care in the community.
“We don’t need anyone’s permission to look after diabetes patients – we just need the resources to do it properly. Currently, it is not being done properly in hospitals. They do not have the resources or time to provide this type of care and they do not really need to be doing it anyway.”
Dr O’Sullivan estimates that around E17 million would have been required to resource general practice properly in the planned integrated diabetes care programme, which he says is a modest investment that would save money for the health system in the longer term.
He believes it inevitable that the fee cuts being imposed will have a deleterious impact on primary care service provision. For example, the reduction in the weighting for a practice’s over-70s patients for PCRS grants to hire staff will reduce practice resources by cutting the level of grants available.
“This will particularly affect practices in deprived areas with a large proportion of medical card patients,” Dr O’Sullivan says.
“With income constantly falling, something will have to give and unfortunately, some of these things may include pro-bono work currently undertaken by GPs.”
College reaction
Dr Peter Sloane, director of the Network of Establishing GPs (NEGs), says the combined impact of the fee cuts and the lack of proper Government engagement with general practice on improving care pathways has led to great uncertainty in the specialty.
He says current economic difficulties have led many older GPs to consider whether retirement at this stage is financially viable. This in turn would limit the career opportunities for younger GPs.
“Most people seem to feel that after the latest FEMPI cuts, general practice is a market that the Government simply isn’t interested in investing in. It appears to be a race to the bottom – an increased volume of patients for reduced income and no investment in general practice infrastructure.”
The current uncertainty, he says, is leading to many younger GPs considering moving abroad.
It seems incredible that the current situation is being presided over by a Health Minister who until recently was himself a practising GP, Dr Sloane says. “One would imagine that someone with a GP background would have insight into the psychological impact of such cuts on general practice.”
He says it would now be a concern that there will be a significant disengagement of general practice as an entity from Government proposals and policies.
“General practice is still a great job and a great career, but it is difficult to see how in the current circumstances a young GP would have the motivation to become established.”
A slap in the face
Cork GP Dr Mary Favier said in her practice, they had been valiantly trying to maintain a reasonable standard and quality of care in the face of the recession and previous fee cuts.
“However, the latest FEMPI cuts are simply a slap in the face,” she says.
Her practice will now have no choice but to cut staff, probably introduce waiting lists, refer more patients on to hospital care, provide less chronic care management and generally cut down on work that no longer pays for itself.
“We just cannot continue to provide the level of service we have been trying to provide.”
For example, the practice will no longer carry out suturing, and will not be able to maintain its already significant diabetes recall service, Dr Favier says.
“Unfortunately, our patients are going to get a rude shock, but we have no alternative. I feel that what is happening at the moment is putting the development of general practice back 20 years.
“It is hard to credit that the Minister is himself a GP. I feel he knows full well what the impact of these cuts will be but is relying on the fact that usually, GPs will always try their best to maintain services.”
She stresses that for practical reasons, this goodwill can no longer be guaranteed.
Dr Favier, who has been deeply involved in College affairs for many years, says the ICGP was completely right to withdraw its representatives from the clinical programmes. “It really is a case of the emperor having no clothes.”
Government policy
College Medical Director Margaret O’Riordan points out that it is Government policy to have a primary care-led health service.
“International evidence supports the fact that primary care-led health services are more cost effective than those led by secondary care. At a time of economic recession the Government should now more than ever prioritise the delivery of services in primary care.
“With an increasingly elderly population, the burden of chronic disease will continue to rise exponentially, placing more and more pressure on the health service. The clinical care programme model offers a way forward and promotes integrated care across the primary/secondary care divide.”
However, Dr O’Riordan says to date, there has been virtually no investment in primary care to support the roll-out of the chronic disease guidelines which have been developed by the clinical care programmes.
“GPs and their staff are currently working at full capacity and cannot absorb further work unless resources are deployed in the community and in general practice. GPs are highly trained specialists who are willing and able to take on structured chronic disease management but need a well-resourced infrastructure to enable them to do so. The way forward is for the Government to truly focus on its commitment to a primary care led health service and work with all health professionals including GPs in order to do so.”
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)