CHILD HEALTH
Trichotillomania leading to a trichobezoar
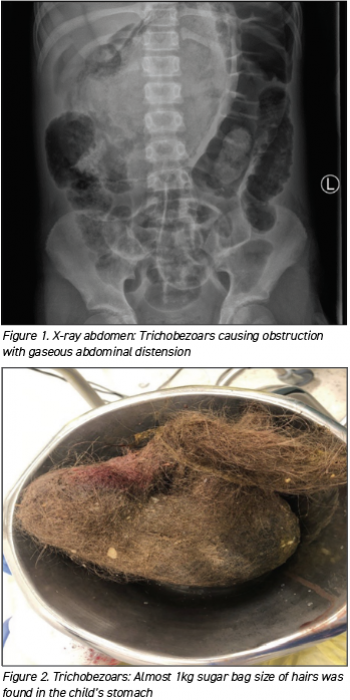
An unusual presentation of acute intestinal obstruction due to a trichobezoar, which resulted in intestinal perforation
July 14, 2023
-
A 12-year-old Girl presented to paediatric ED at night with acute onset of abdominal pain and persistent vomiting for the past eight hours. There was no blood, mucous or bile stain in her vomit. She was unable to tolerate anything orally and had persistent abdominal pain. She was triaged as category 3, and was reviewed by the paediatric team initially, for vomiting and abdominal pain in the paediatric ED.
She had her all vaccinations and had an allergy to amoxicillin, with a history of rashes in the past. She was in main stream school, with normal developmental history but there were some concerns of Asperger’s syndrome, for which she was awaiting an assessment. She was vitally stable on presentation with a heart rate of 105, BP: 114/77, respiratory rate: 22 and she was afebrile.
On examination two hours after presentation, her condition had worsened; she was weak, lethargic and her appearance was pale with a capillary refill time of two to three seconds, and dry mucous membrane. She had tachycardia with normal BP. She had shallow breathing with marked abdominal distention generalised tenderness and positive bowel sounds. Other systemic examination was unremarkable. The child was also noted to have a high pain threshold on examination. Clinically she was noted to have acute abdomen pain, likely due to a large bowel obstruction or volvulus.
Investigations
This patient was started on intravenous fluids bolus and given triple antibiotics after obtaining baseline bloods including FBC, U&E, LFT, amylase, CRP and VBG and blood culture. She was kept NPO and the surgical team was contacted for urgent review. Her VBG had pH: 7.35, pCo2: 4.9, pO2: 9.8, glucose: 10.9, lactate: 2.1, WBC: 3.7, neuro: 2.59, lymph: 1.05, HB: 13.6, CRP: 5, normal electrolytes and liver functions.
Abdominal x-ray obtained after two hours of presentation showed dilated large bowel loops at uneven areas, which suggested acute intestinal obstruction or volvulus. The patient was then reviewed by the surgical team. A CT abdomen was preformed, which showed marked distension and filling of the stomach with heterogeneous material, suggestive of gastrointestinal (GI) bezoars. There was evidence of acute hollow organ perforation with large amount of free fluid and free air in the abdominal cavity. She was transferred urgently to tertiary care for open laparotomy.
Open laparotomy was performed on the same day with almost 1kg (sugar bag size) of hairs found in her stomach. Resection anastomosis repair was carried out for the perforation, the patient needed inotropes in ICU on day two of surgery and was moved to a ward on day five post surgery. She spent three weeks in hospital and was later discharged home.
 (click to enlarge)
(click to enlarge)
