CHILD HEALTH
PHARMACY
Use of antipyretics in children
Educating parents on the proper dosage of antipyretics could reduce the number of re-visits to emergency departments and primary care
December 1, 2012
-
A large number of consultations take place on a daily basis in general practice involving the management of febrile illness in young children. It is frequently noted by primary care practitioners that a large proportion of parents do not understand how to manage fever correctly in their child, particularly when it comes to the administration of antipyretic medication. Parents often make mistakes in dosage and frequency of administration of antipyretics.
It is common knowledge that in the paediatric hospital setting, antipyretic medications are generally administered according to the weight of the child, as opposed to their age. In the community setting however, antipyretics are administered as per the age of the child, as this is what parents are instructed to do according to the paracetamol/ibuprofen containers. Because of this, many children are undertreated and remain pyrexial, leading to more frequent emergency department presentations.
The aim of my study was to assess the usefulness of an information handout for parents on the use of antipyretic medication in their child, which allowed for the antipyretic dose to be calculated by the weight of the child as opposed to the age.
Literature
The existing literature shows that parents frequently make errors in dosage and frequency of antipyretics administered to their children. A large proportion of parents will administer the medications in too high, too low, too frequent or infrequent doses.
Many parents administer antipyretics even when there is minimal or no fever because they are concerned that their child must always maintain a ‘normal’ temperature. Overdosing may cause drug toxicity, while underdosing may lead to unnecessary repeated GP visits.
It has also been noted that many doctors have a significant lack of knowledge on the correct use of antipyretic agents in children. There is evidence that clear guidelines on correct antipyretic dosing would be beneficial.
It has been found that pyrexia is the primary complaint of one-third of patients seen in paediatric emergency departments and there is clear evidence that many parents wouldn’t attend an emergency department if their child’s fever subsided at home, after using the correct antipyretic treatment.
Weight vs age
In regard to the issue of weight as opposed to age, the Italian Paediatric Society Guidelines of 1999 clearly state that antipyretic dosage should be based on a child’s weight rather than age. An article published in January 2010 on childhood obesity reported that in 2005, over 300,000 Irish children were overweight or obese and figures have since risen. 1
Clearly, now more than ever, with the weight of the average child on the increase, amendments need to be made to ensure medication administration is weight based as opposed to age based.
Paracetamol/ibuprofen
Prior to developing the handout, I also decided to look at the commonly used antipyretic agents today. Most of these agents make recommendations on dosing as per the child’s age. Firstly I looked at a particular brand of liquid paracetamol. Up to November 2011, if one followed the instructions provided, a one-year-old child received the same dose as a six-year-old. Now thankfully, the age bracket has been narrowed, so there is now a six to 24-month, a two to four-year and a four to six-year age dosing bracket.
However, I’ve found that even with these updates, there are still issues. If you take for example an average three-year-old male who weighs 16kg, as per his weight he should receive 10ml of the liquid, but as per his age he only receives 7.5ml. So even if parents follow the recommended instructions correctly, often a child could receive 25% less antipyretic than they should as per their weight. And this is only in relation to the average-sized child. For those children above average weight, the discrepancy is even greater.
The same applies to the administration of ibuprofen. The discrepancies aren’t as great as seen with paracetamol; however, on average a child should receive 10-20% more ibuprofen if the dose is calculated per weight.
These may all seem like small discrepancies, but those additional few millilitres of antipyretic may be all that is needed to control pyrexia in a child and hence reduce re-presentation of that child to primary care or the emergency department.
Methodology
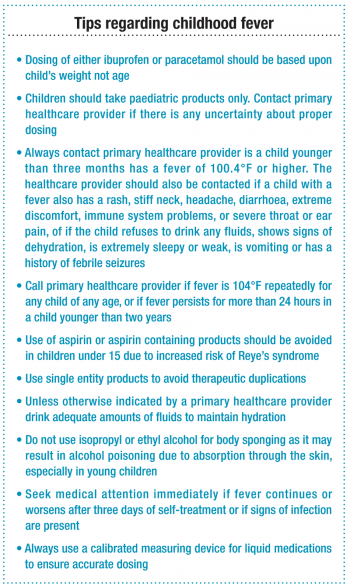
A two-page handout was devised for use by in primary care in consultation with the parent of a pyrexial child. The first page was for the healthcare practitioner only. It outlined which children the handout was suitable for, ie: distressed children aged from six months to six years with a pyrexia greater than or equal to 38°C. It also briefly outlined the verbal information that should be provided to parents when the handout was being distributed.
It then allowed for calculation of the correct dosage of paracetamol and ibuprofen using the algorithms provided, as per the weight of the child (paracetamol at 15mg/kg and ibuprofen at 7.5mg/kg).
The second page of the handout was for the parent to take home. It consisted of a 24-hour table in three sections: one each for paracetamol, ibuprofen and an antibiotic (if prescribed). It allowed for the dosage of antipyretics as per the child’s weight to be filled in at the required times of administration over a 24-hour period (as well as an antibiotic). Once the table is filled in by the primary care practitioner, it is signed and dated and mum or dad takes it home with them.
The handout was used by myself and the other GPs in the practice for four weeks beginning on November 14, 2011. Four to five days after initial presentation, I contacted each parent and asked them 10 questions in relation to the handout and pyrexial management in their child. In total, 40 handouts were distributed in that time. All of the parents were contactable for the follow-up telephone questionnaire and none of the results were excluded from analysis.
Results
Almost 66% of parents had only one child, while only 5% had four or more children. Some 40% were between the ages of one and two years. Almost 90% were under three years of age. A total of 60% of parents thought that antipyretics should be administered at ≥ 37°C. Only 10% had been aware that antipyretics could be calculated as per the weight of the child. The next question revealed that 35% of parents did not know that both paracetamol and ibuprofen could be used to reduce fever. The majority knew that paracetamol could be used, but not ibuprofen.
Prior to receiving the handout, 20% of parents were not aware that they could use paracetamol and ibuprofen in conjunction with an antibiotic. A total of 37.5% of these thought that antipyretics were not needed as the antibiotic would reduce the fever, while 62.5% thought that it would be a danger for their child to have antipyretics and antibiotics in conjunction with one another.
Of the parents who received the handout, 97.5% used it. One parent did not use it as her child’s fever resolved soon after she left the surgery. All 39 parents who used the handout found it useful. The majority of parents thought the handout was easy to follow; they said it helped to reduce their anxiety levels regarding their child’s fever and they liked the way the handout was individualised to their child.
Of the 40 parents who took part in the study, only one re-presented to the practice with their child in the days following their initial presentation. The reason for this was that their child developed a rash that the parent was concerned about. None of the children presented to an ED in the days following their initial presentation.
A total of 62.5% of parents felt that their primary care practitioner generally doesn’t spend enough time educating them about pyrexia management in their child; with 15% saying that they often felt anxious when leaving the surgery.
 (click to enlarge)
(click to enlarge)
