NUTRITION
Care of the stroke patient
A new guidance document has made key recommendations around nutrition and hydration in stroke patients
August 29, 2019
-
Malnutrition and dehydration rates after stroke are high. Malnutrition affects up to a quarter of patients in the first weeks after stroke, and the risk of malnutrition may increase to up to 49% over the course of their hospital stay.1,2,3 Dehydration may affect up to 62% of patients following a stroke.4 Physical, social and psychological elements play a key role in this due to factors such as dysphagia, reduced ability to self-feed, cognitive impairment, anxiety or depression, unfamiliar foods and fatigue resulting in a reduced intake of food and fluids.1
Poorer outcomes are found in patients with malnutrition/dehydration following a stroke, with malnutrition associated with reduced functional improvements, increased complication rates and prolonged hospital length of stay.2,4,5,6
However, early identification of malnutrition risk and implementing individualised nutrition care plans for patients with stroke can improve nutritional status and functional outcomes, while reducing complications and length of hospital stay.2,4,5,6,7
Dysphagia is another important factor to consider in the nutrition and hydration care of stroke patients. Dysphagia is an eating, drinking and/or swallowing disorder, usually caused by a neurological or physical impairment of the oral, pharyngeal or oesophageal mechanisms.8 It can significantly impact on both dietary and fluid intake, increasing the risk of malnutrition and dehydration.5 Up to 78% of patients following a stroke may experience dysphagia.9 Aside from malnutrition, other physical consequences of dysphagia can be severe, ranging from aspiration and choking to death.10
New guidance document
The National Clinical Programme for Stroke was established in early 2010. At the end of 2016, the programme identified a gap in standardised care around nutrition and hydration in stroke patients in Ireland. A multidisciplinary working group was formed in 2017 to develop evidence-based nutrition and hydration recommendations to promote best practice for people with stroke. After an extensive review process of national and international guidelines by the working group and consultation by relevant bodies, Recommendations for the Management of Nutrition and Hydration in Patients with Stroke – a Guidance Document was published in April 2019.
These recommendations were produced to support all healthcare professionals, support staff and students to provide the best nutritional care for stroke patients in order to achieve better outcomes. This document is split into different categories with evidence-based recommendations clearly outlined at the end of each section.
Some key recommendations of particular interest to dietitians are described below (for recommendations in full, see the original guidance document at:
www.hse.ie).Screening recommendations:
- All patients should have a swallow screening completed within four hours of admission and before taking any food or fluids orally
- All patients should be screened for malnutrition within 24 hours of admission to a healthcare setting, using a validated screening tool and repeated at least weekly thereafter in the acute setting, and as indicated by risk scores in rehabilitation, community and care home settings
- All stroke patients should be monitored for self-feeding deficits and if any identified, should receive an assessment by an occupational therapist.
Hydration recommendations:
- Risk of dehydration should be considered within four hours of admission with immediate consideration for alternative fluids until a safe swallow method is established
- Regular monitoring of fluid balance and electrolytes in those with severe stroke or swallowing difficulties
- Patients requiring thickened fluids should be considered for alternative fluids, if appropriate, based on hydration status.
Dietetic referral recommendations
All of the following should be referred to a dedicated stroke dietitian for specialised individualised assessment, advice and monitoring:
- Malnourished or at risk of malnutrition
- Unable to take adequate nutrition and fluids orally
- Dysphagia patients who require texture modified foods or thickened liquids
- Patients who require tube feeding
- Nutrition-related comorbidities, ie. diabetes, components of the metabolic syndrome, constipation, pressure ulcers, falls, renal failure
- Modifiable secondary prevention risks including hypertension and hyperlipidaemia.
Oral nutrition support recommendations:
- Oral nutrition support should be considered for patients who can swallow safely and are malnourished or at risk of malnutrition
- Oral nutritional supplements (ONS) may be considered for patients who are at risk of malnutrition if there is concern about the adequacy of oral nutritional intake. There is no evidence for the routine use of ONS for patients following a stroke
- A complete oral multivitamin and mineral supplement (providing the recommended daily allowances for all vitamins and trace elements) should be considered if there is concern about the adequacy of micronutrient intake. There is no evidence for the routine use of multivitamin and mineral supplements for those following a stroke.
Enteral nutrition support recommendations:
- People with acute stroke who are unable to take adequate nutrition and fluids orally should be:
– Considered for nasogastric (NG) feeding within 24 hours of admission with commencement of NG feeding within 48 hours
– Considered for a nasal bridle, if the NG tube requires frequent placement, using locally agreed upon protocols
– Considered for gastrostomy tube if unable to swallow adequate food and fluids orally by four weeks from onset of stroke, need but are unable to tolerate nasogastric tube feeding with nasal bridle or are at high long-term risk of malnutrition
- All stroke units should have an out-of-hours enteral feeding regimen in place (criteria for consideration in an out-of-hours feeding regimen and an example of an out of hours regimen are included in the guidance document)
- All stroke patients on enteral feeding should be able to access dietetic services independent of the location of their care (acute inpatient, inpatient rehabilitation or community-based services).
Parenteral nutrition support recommendations:
The parenteral feeding route should only be used if the gastrointestinal tract is not functioning effectively and/or all enteral nutrition options have been considered and excluded at that point, including nasal bridle and percutaneous endoscopic gastrostomy (PEG) placement.
Ethics recommendations:
- Decisions regarding the use of artificial nutrition and/or hydration should be made on an individual patient basis after meaningful discussion by key members of the multidisciplinary team
- Clear and regular communication with the patient, if possible, and their family is essential to ensure the patient’s wishes are known, any perceived concerns regarding dehydration or lack of nutrition are discussed and that a clear plan is in place.
Secondary prevention recommendations:
- All patients with modifiable risk factors (hypertension, overweight/obesity, suboptimal diabetes control, new diabetes diagnosis and hyperlipidaemia) should be offered specialist dietetics counselling on risk-reduction strategies.
- Pathway to standardise nutrition and hydration care in patients with stroke
- A clear visual pathway was also developed to support these best practice recommendations (see Figure). This can be used in any setting and audited on a yearly basis to measure the success of its implementation and strive to achieve the highest and safest standard of nutrition and hydration care for stroke patients.
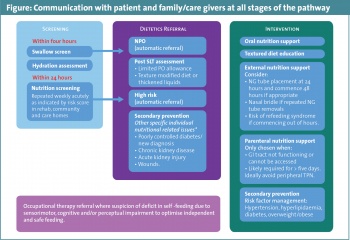 (click to enlarge)
(click to enlarge)
