DIABETES
GERIATRIC MEDICINE
Challenges in treating an ageing population
Treating older people with diabetes who may be frail, living in nursing homes and possibly with multimorbidity can be truly complex
July 1, 2015
-
In the Republic of Ireland, 2.8% and 11% of the population is comprised of people aged ≥ 80 years and ≥ 65 years respectively.1 These values are projected to increase by 2030 to 4.3% and 16%.1 It is estimated that about one-third of residents that are admitted to nursing homes have type 2 diabetes2 and approximately 4,000 patients > 65years of age currently reside in long-term care in the Republic of Ireland.1
Diabetes presents specific complex issues. It is a multisystemic chronic disease that results in microvascular and macrovascular complications such as retinopathy, renal disease, neuropathy, stroke, coronary artery disease, and peripheral vascular disease.3
Older people with increased frailty and comorbidity are more susceptible to diabetic complications. Hence, the management of type 2 diabetes in the elderly residents in nursing homes can pose a unique challenge. Current guidelines advocate for individualised care plans and an interdisciplinary team approach in this population.4,5
In this article, the complexity of type 2 diabetes management in the elderly population in nursing homes and the need for individualised care plans is discussed. In addition, a case study highlighting this complexity is presented and the existing guidelines are described.
The complexity of diabetes in frail elderly and those resident in nursing homes
Type 2 diabetes is complex in the elderly population as it is characterised by increased risk of comorbid diseases, functional deterioration and clinical frailty.4 Comorbidities are more common in the elderly with studies showing that 40% have at least three illnesses.4
This cohort is more susceptible to the adverse effects of drug interactions and polypharmacy. Residents admitted to nursing homes frequently present with type 2 diabetes and one or more acute illnesses, such as congestive cardiac failure, infections, fractures, stroke and pulmonary diseases. Therefore, they are at increased risk of short-term and atypical complications of diabetes, such as falls, dehydration, poor wound healing, skin ulcers, weight loss, urinary incontinence, and pain syndromes, all of which can result in poor quality of life and poor health outcomes.2,6
Cognitive impairment is more prevalent in elderly patients. In a cohort study in 2010, people with dementia were found to have mortality rates increased three-fold compared to those without dementia in the first year after diagnosis and increased two-fold from the second to the sixth year after diagnosis.7
Patients with cognitive impairment are three times more likely to develop severe hypoglycaemia.8 Dementia is progressively being linked to type 2 diabetes as a cause and complication.6 As a result, it plays an important part in determining the optimum diabetes care plan for the affected person.
A quarter of elderly patients with type 2 diabetes are frail.4 Frailty is a syndrome characterised by loss of energy, cognition, physical ability and health that results in vulnerability.9 Clinical frailty can be used in the development of interventions and services an individual may require. In addition, it can aid in the prediction of mortality risk and need for long-term care.9
The Canadian Study of Health and Aging (CSHA) Clinical Frailty Scale is a 7-point scale that evaluates frailty taking into account comorbidity, functional disability and cognitive impairment.9,10
This scale can be utilised in establishing degree of frailty which in turn will aid in creating an individualised diabetes care plan.
This Clinical Frailty Scale can be utilised in establishing degree of frailty which in turn will aid in creating an individualised diabetes care plan.
Managing the elderly population with type 2 diabetes
Several studies have demonstrated the range of comorbidities and functional impairment in older adult populations. They highlighted significant characteristics which include increased risk of hypoglycaemia, recurrent hospitalisation and development of cognitive impairment and frailty.
These features were taken into consideration in the recommendations of the clinical guidelines for type 2 diabetes management in the older population by the International Diabetes Federation.4 The guidelines recommend individualised care plans tailored to the specific features of the elderly patient with type 2 diabetes and the employment of an interdisciplinary approach.
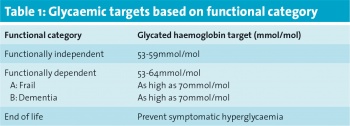
Patients have been stratified into three main categories:
• Category 1 is functionally independent (full mental capacity to self-manage their diabetes and reasonably healthy)
• Category 2 is functionally dependent (have some loss of function)
• Category 3 is end of life care.
The functionally dependent category 2 is further divided into subcategory A – frail and subcategory B – dementia (those with some degree of cognitive impairment and who are unable to self-manage their diabetes).
The emphasis of management of diabetes in older people is on achieving glycaemic levels that prevent and reduce vascular complications as well as reducing the risk of hypoglycaemia. Glycaemic targets should be individualised based on comorbidities, functional status, history of risk of hypoglycaemia, presence of micro/macrovascular complications and cognitive impairment. Table 1 shows the glycaemic targets based on functional category.
 (click to enlarge)
(click to enlarge)
