GASTROENTEROLOGY
NURSING
Constipation: Roughage to regulate
Constipation can negatively impact on quality of life and cause many to silently suffer
September 1, 2013
-
Constipation is widely prevalent in the western world and its incidence varies from 2-30%.1 Worldwide figures indicate that approximately 12% of the population experience constipation.2 It affects people of all ages, but is more common in children, the elderly and pregnant women.3
Constipation is a condition in which bowel evacuations occur infrequently or in which the stools are hard, small and where its passage causes difficulty or pain.4 The Bristol stool chart is often used in residential care settings to help diagnose constipation, with type 1 or type 2 stool formations indicating constipation.
The frequency of bowel evacuation varies greatly from person to person, so defining what is ‘normal’ is difficult. A reduction in the frequency and/or a harder consistency of bowel movements developing in a person of previous regular bowel habit is likely to indicate constipation.
Causes
The causes of constipation can be categorised into either primary or secondary constipation. The most common cause is primary and relates to inadequate dietary fibre intake, poor hydration, reduced mobility or conscious retention of faeces.
Secondary constipation can originate from many different disease states or as a side-effect of medications.5 Common conditions contributing to the development of constipation include: intestinal obstruction from tumours or hernias; metabolic alterations such as hypokalaemia; endocrine disorders such as hypothyroidism; or neuropathic disorders such as Parkinson’s disease or multiple sclerosis.3
A plethora of medications can result in constipation, including antacids, antihistamines, antipsychotics, some antidepressants, calcium and iron supplements, diuretics and opioids. Although constipation is rarely serious, it can lead to bowel obstruction, chronic constipation, haemorrhoids, hernia, irritable bowel syndrome and laxative dependency.6
Constipation in children
Constipation in children is common, affecting up to 30% of the child population. It ranks second in terms of most referrals received from paediatric gastroenterologists.7 It can be a distressing problem for the child and their family, however, parents should realise that every child is different and what is ‘normal’ can vary greatly. A change from what is normal for a particular child may suggest a problem.
Constipation can occur at any age in children but occurs more often when weaning and potty training, at four months and two years respectively.3
It can sometimes occur due to an underlying disease or condition such as hypothyroidism, cystic fibrosis, and some neurological conditions. Meanwhile, idiopathic constipation occurs when no particular disease or illness is the cause. This type of constipation is most common.
The discomfort and distress of a child during a bout of constipation can increase their likelihood of refusing to defecate in the future and lead to the intentional withholding a stool, resulting in a greater risk of impaction (ie. overflow diarrhoea).
Regular soiling may indicate that a child has constipation with impaction. In addition to deliberately holding a stool, other causes include: poor intake of dietary fibre and fluid; emotional disturbances; and changes in routine.8 Early identification and effective treatment can greatly improve outcomes for children.
Evidence-based guidelines were developed by the National Institute for Health and Clinical Excellence (NICE) in 2010 giving key recommendations in the treatment and management of idiopathic constipation in children:7
- The first-line treatment crucial for dis-impaction is prescribing the correct dosage of laxatives, which should be reviewed a week after commencement
- Once faecal impaction has been cleared, laxatives should be prescribed as maintenance therapy to help the child establish a regular bowel habit. This may take some months to ensure that impaction does not build up again and become a chronic problem
- Dietary intervention alone is not recommended as a first-line treatment of impaction in children, but advice should be given on eating the right food and drinking enough fluids (six to eight cups a day)
- Children should be encouraged to take time to go to the toilet, and to develop a good daily pattern of toilet habits. It can also help if parents keep a bowel diary, recording their child’s bowel movements and rewarding them with a positive attitude when they use the toilet.
Constipation in the older person
Older people can be more prone to constipation than the general population due to several factors. A large proportion of the elderly population, in particular those in long-term care, tend to have reduced mobility levels which can contribute to reduced gut motility. They are also known to have a lower intake of dietary fibre and fluids in comparison to younger adults.
Many are on numerous medications, some of which will have the side-effect of constipation, and many have developed disease states which can result in secondary constipation.
Constipation during pregnancy
Most women will experience constipation during pregnancy. This can be due to a potential decrease in physical activity, dietary changes, iron supplementation, and the physiological effects of pregnancy on gastrointestinal function.3
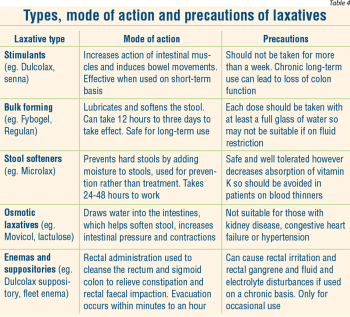
Pregnant women may also intentionally restrict their fluid intake to reduce their urge to urinate frequently. Measures that may alleviate constipation in this group include increasing fibre and fluid intake, changes in the type of iron supplement, and if necessary, using faecal bulking agents (see Table 4).
How can fibre benefit health?
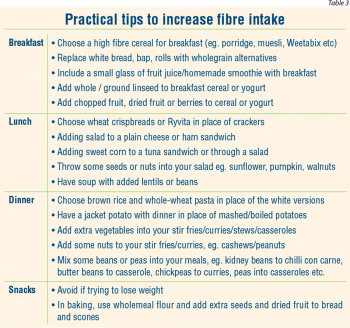
Fibre, also known as ‘roughage’, is the part of the food that is not digested by the body. It is only available from foods of plant origin such as unrefined cereals, wholemeal flour, fruit, vegetables, nuts, seeds and pulses such as peas, beans and lentils. As fibre passes through the bowel it absorbs and retains water, which creates bulk and leads to regular bowel habits.9
Studies show that including fibre in the diet holds additional benefits to boosting digestive health. A diet rich in wholegrain and high-fibre cereals may prevent or control diseases such as heart disease, diverticulitis, type 2 diabetes, and bowel cancer. It combats fatigue, enhances mood, and can help manage weight by adding bulk to the diet, containing few calories and helping us to feel fuller for longer.10,11,12
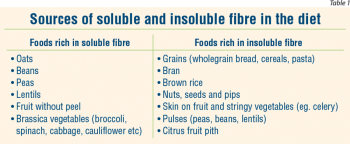
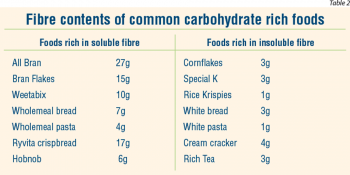
There are two main types of fibre: soluble and insoluble. Soluble fibre dissolves in water and is digested by the bacteria in the colon, releasing gas. It is a viscous, gel-like fibre, which helps lower cholesterol levels in the blood. It slows the absorption of glucose, which is important for those at risk of or with diabetes.
Insoluble fibre does not dissolve in water, but absorbs up to 15 times its weight in water, swelling like a sponge.12 It is not digested by colonic bacteria and is excreted in the stools (see Table 1).
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)