CARDIOLOGY AND VASCULAR
Diagnosis of syncope and review of link with vitamin deficiencies
Using tilt table testing, a team at Midland Regional Hospital, Tullamore reviewed diagnostic outcomes in patients with syncope and investigated associated vitamin D and B12 deficiencies
December 8, 2017
-
Syncope is a clinical syndrome in which transient loss of consciousness (TLOC) is caused by a period of inadequate cerebral nutrient flow, most often as a result of an abrupt drop of systemic blood pressure. Typically, the inadequate cerebral nutrient flow is of relatively brief duration (8-10 seconds) and in relation to syncope it is by
definition spontaneously self-limited.Tilt testing is recommended where a cardiac cause of syncope has been outruled. It helps to differentiate between both orthostatic hypotension (OH) and reflex syncope as well as syncope occurring with jerk-like limb movements and epilepsy. Reproduction of symptoms here is diagnostic.1 Vitamin B12 is implicated in causing autonomic dysfunction and hence is an important cause to rule out when assessing a patient with orthostatic hypotension and syncopeal symptoms.2,3,4,5,6 Vitamin D is also known for causing orthostatic hypotension according to recent studies and its deficiency is very common in the general population, making it an important reversible cause of syncope due to OH.7,8
The syncope unit in Midland Regional Hospital, Tullamore accepts patients who have being referred by their GP or are admitted to hospital for investigation of unexplained falls and syncope. The tests performed can include a head up tilt (HUT) and/or active stand (AS), prolonged tilt (PT) and carotid sinus massage (CSM).
Objective and method
The purpose of this study was to review diagnostic outcomes in patients’ syncope or pre-syncope through the use of tilt table testing, and to find the co-relation of its association with vitamin D and vitamin B12 deficiency after ruling out other causes of the symptoms.
This is a retrospective analysis of haemodynamic changes in response to tilt table testing, which were recorded by a non-invasive volume clamp technique (finometer). The following diagnoses were made:
- Orthostatic hypotension (OH)
- Carotid sinus syndrome (CSS)
- Neurocardiogenic syncope (NCS)
- Postural orthostatic tachycardia syndrome (POTS).
- Blood levels of vitamin D and vitamin B12 were then checked.
Results
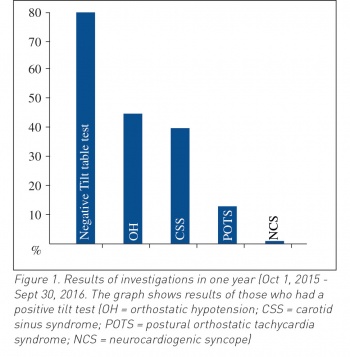
A total of 181 patients underwent investigation during a one year period from October 1, 2015 to September 30, 2016. The mean age of patients was 72 years and the male to female ratio was 1:1.9. Out of 181 patients, 100 of them had positive tilt table test. Out of the 100 patients with positive tilt table test, 46% (n = 46) met the criteria of OH. The mean systolic drop in blood pressure was 40mmHg and the mean diastolic drop was 20mmHg.
Out of these 40% (n = 40) were diagnosed with CSS on the basis of spine and erect CSM manoeuvre, with 27.57% (n = 31) of these being vasodepressor and 13.29%( n = 9) being cardio-inhibitory. A total of 13% (n = 13) were diagnosed with POTS, all of whom were females. One patient from the investigation was diagnosed with NCS.
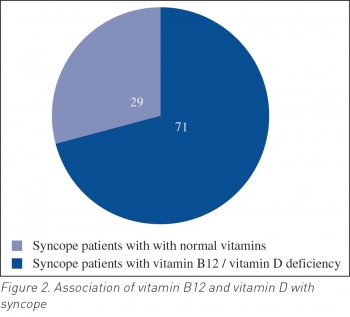
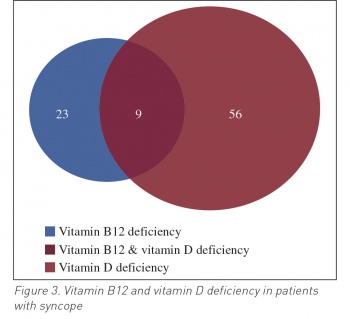
Out of these 100 patients, 71 had vitamin B12 or vitamin D deficiency. Hence, only 29 patients had normal vitamin levels (see Figure 2). A total of 23% (n = 23) patients with syncope were vitamin B12 deficient; out of these 12% (n = 12) were diagnosed as OH and 9% (n = 9) with CSS, while 2% (n = 2) were diagnosed with POTS.
On the other hand 56% (n = 56) of patients with syncope had vitamin D deficiency, 24% (n = 24) of patients with CSS were deficient in vitamin D, 22% (n = 22) had OH and 12% (n = 12) were given the diagnosis of POTS. Nine patients had a deficiency of both vitamin D and vitamin B12. A total of 34 (60%) of the 56 patients with vitamin D deficiency and 13 patients (58%) with vitamin B12 deficiency were female with syncope diagnosed by tilt table testing (see Figure 3).
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)